Scores




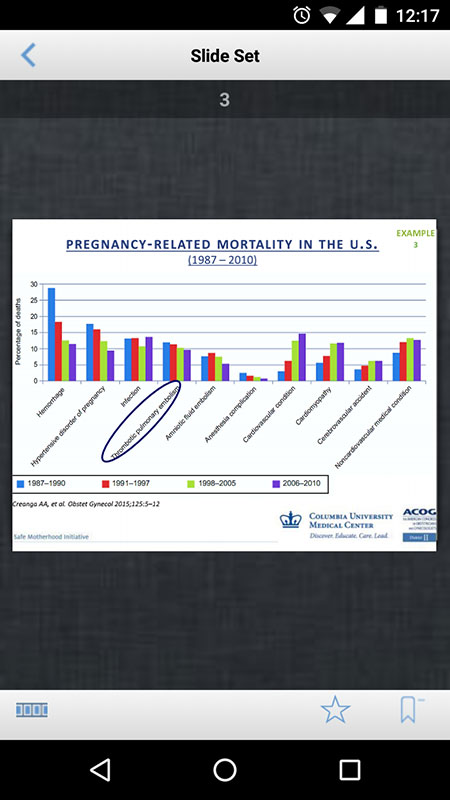
The 20th century saw a rapid decline in maternal deaths in the United States. However, this trend reversed in the late 80s, when a study has shown a steady rise in maternal deaths across the country.
A follow-up study of maternal mortality trends in 181 countries, from 1980 to 2008, further confirmed that this increasing trend had been unique to the US, as much of the world had instead been experiencing declines in maternal deaths.
The U.S. had 2006 maternal mortality ratio (MMR) of 13.3 maternal deaths per 100,000 live births, which means the country did not achieve the Healthy People 2010 goal of 4.3 maternal deaths per 100,000 live births.
The most recent study on global maternal mortality showed that the U.S. had an MMR of 18.5 per 100,000 live births, which is the highest among all developed countries in the world.
The U.S. is also one of only eight countries that experienced increases in maternal deaths between 2003 and 2013, with Afghanistan, Belize, El Salvador, Guinea Bissau, Greece, Seychelles, and South Sudan.
Recent trends in maternal mortality in New York State and NYC have also been grim. According to the most recent data from the New York State Department of Health, the 2013-2015 MMR was 20.7 per 100,000 live births for NYS overall, 22.6 for NYC and 18.9 for NY outside NYC, with a higher maternal mortality rate among Black populations (54.6 per 100,000 live births).
Key risk factors behind high maternal mortality ratios include obesity, pre-existing chronic health conditions (most commonly hypertension and cardiac conditions), and advanced maternal age (women 35 years of age and older), as well as disparities in preconception health status and access to care, and underlying structural and health-related factors associated with poverty, racism and its attendant stresses.
The leading causes of pregnancy-related death are hemorrhage, hypertensive disorders, and embolism. The 2012-2013 case reviews found that hypertensive disorder complications during labor and delivery were present in 30% of cases, meaning they are still a significant factor in mortality cases.
As a part of the efforts to tackle this problem, in 2013, the American College of Obstetricians and Gynecologists (ACOG) District II, serving New York, re-launched the Safe Motherhood Initiative (SMI), a voluntary program, that empowered 117 hospitals involved in the care of pregnant women to work together to prevent maternal death and delivery complications.
The SMI examined the research and evidence-based best practices related to the prevention of the leading causes of maternal death: obstetric hemorrhage, severe hypertension in pregnancy, and venous thromboembolism (VTE).
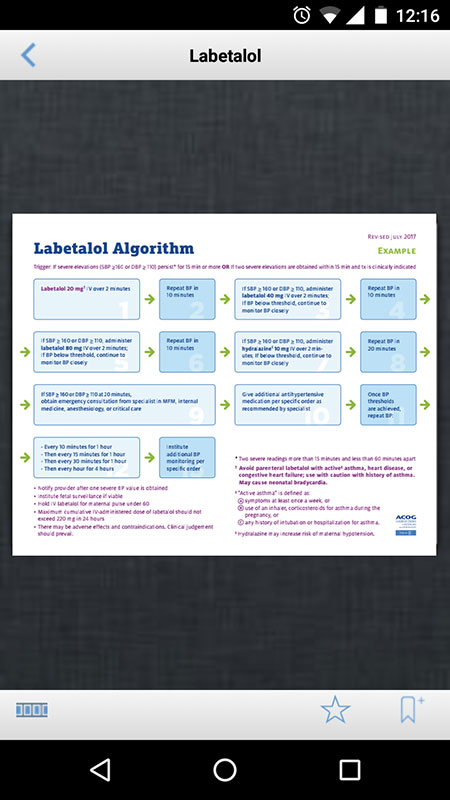
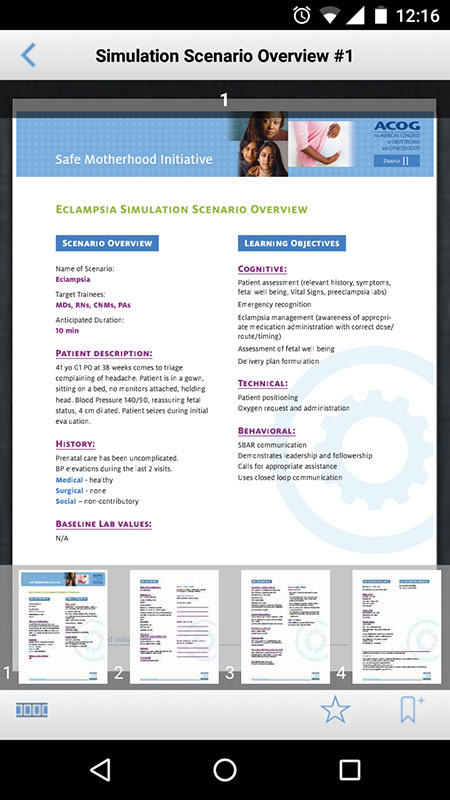
As a result, three safety toolkits or "bundles" were developed, one for each of the three conditions, to provide care guidance, protocols, algorithms, checklists, and other tools to address the needs of any birth facility and obstetric team managing the three identified high-risk conditions.
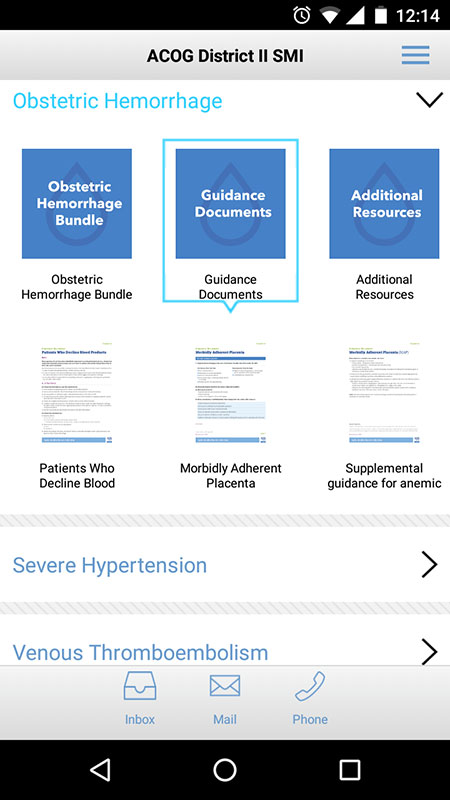
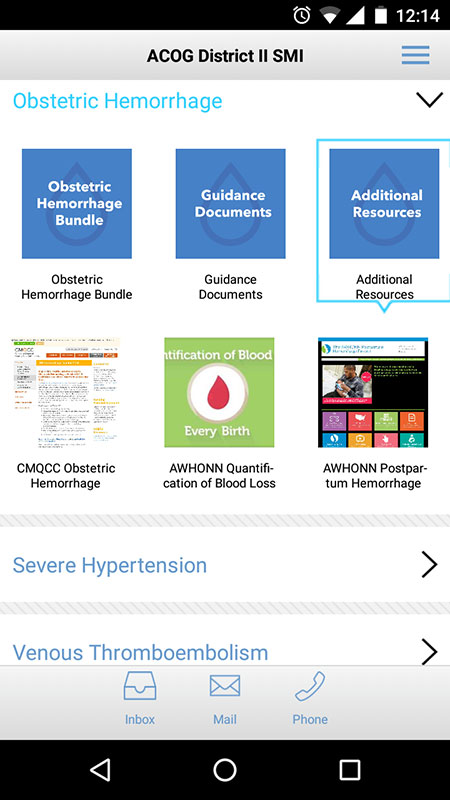
The SMI bundles are available on the ACOG website and downloadable in the Safe Motherhood Initiative app, which is available for Android and IOS devices for free.
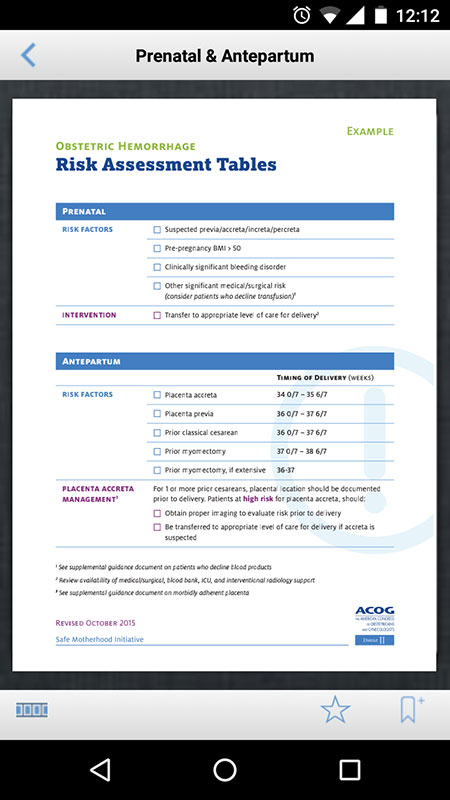
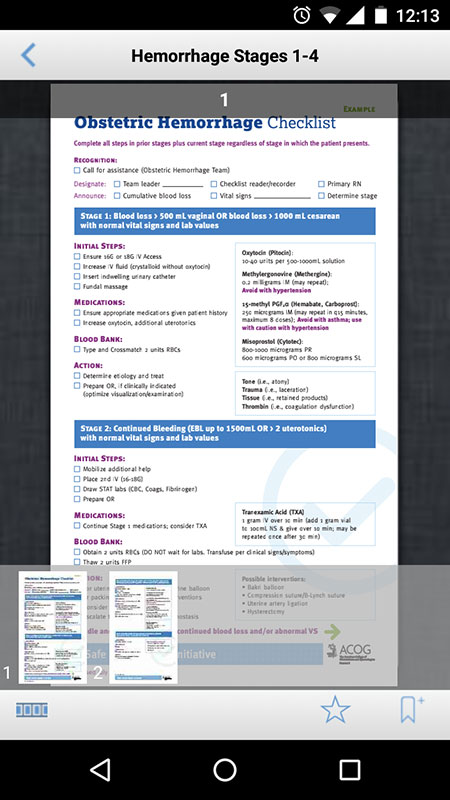
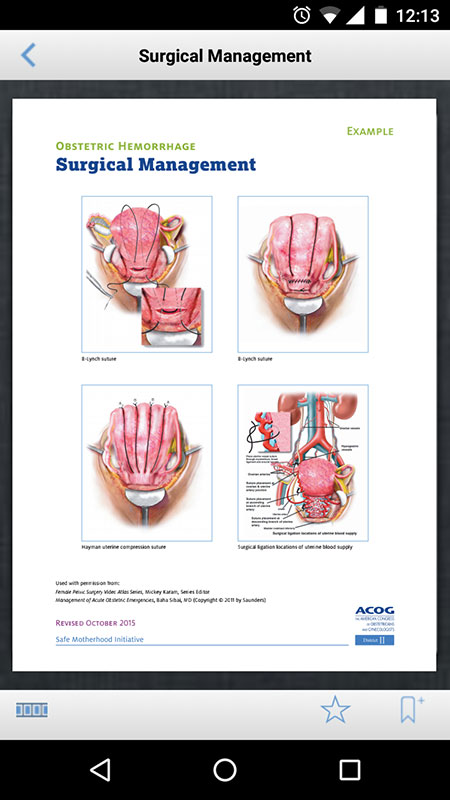
The app brings all of the SMI's materials on mobile devices, including risk assessment tables, checklists, algorithms, clinical presentation slide decks, and guidance documents.
Upon the first launch, that SMI app would try to refresh the content, i.e. download the updates. An Internet connection is required for this, as well as for accessing much of the material, so keep it in mind to avoid unnecessary costs.
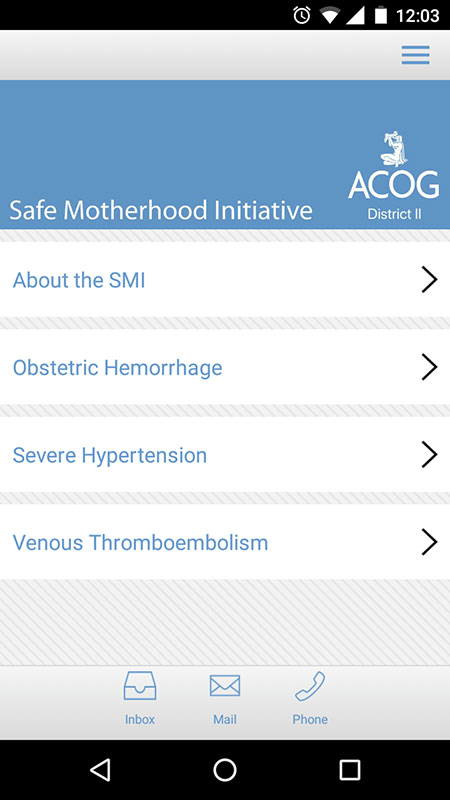
The app's Homepage is simple with four sections on it, including the general About the SMI section, as well as three bundles for each of the conditions.
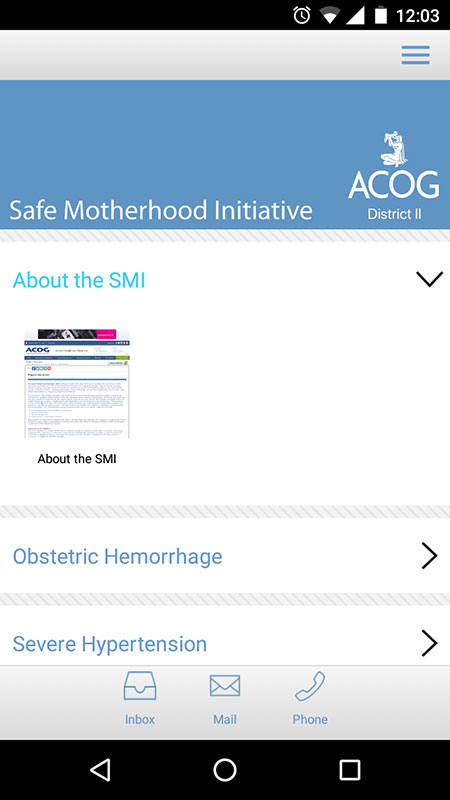
Tapping on the name of the section, expands the section, revealing the materials which are available in a document (PDF) format or in form of slides, except the About the SMI section which is basically the ACOG website adapted to mobile view.
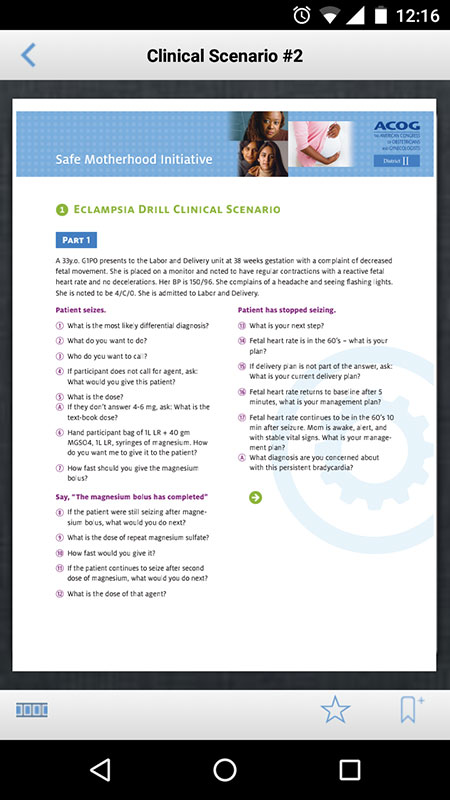
The information in the bundles includes risk assessment tables, checklists, algorithms, educational slides, expert guidance documents, case scenarios, videos, and additional resources, all targeted at the top 3 most common causes of maternal mortality. The information in the app is supported by evidence-based medicine, clinical practice guidelines and standard of care medical practice.
The app is easy to use and follow, however, there's a problem with the navigation, i.e. if you tap on the Back icon in certain section or document, you won't be returned to the previous screen, but to the Home page with all bundles closed.
Also, it could be a problem to view the document and information on smaller screens (there's no option to make it bigger or download it).
Content can be rated and the most frequently viewed resources can be bookmarked for easier access. Users can also search the app for particular topics, however, the Search feature doesn't work so well.
Another problem is a number of obstetric emergencies covered. I think it would be good if the app covered more obstetric emergencies.
Despite this, the Safe Motherhood Initiative app is still a very useful set of bundles that target a growing problem of maternal mortality.
The app compiles the most current evidence-based recommendations from ACOG on the 3 most common causes of maternal mortality, including obstetric hemorrhage, severe hypertension in pregnancy, and venous thromboembolism, bringing them into one resource that can be used at the point of care, i.e. during prenatal visits and in the labor room.
Benefit: The app was designed for Ob/Gyn, midwives, family medicine and emergency medicine providers, and any provider who performs obstetrics
Verdict:
For- The evidence-based recommendations from ACOG
- Includes checklists, algorithms, and risk assessment tables that can be easily reviewed at the point of care
- Useful educational resource for obstetric emergencies
- Requires Internet connection for most of the materials
- Back button makes a navigation frustrating
- Search feature doesn't work as it should
- Some resources are difficult to view on smaller screens












Your thoughts on this
Loading...