Scores




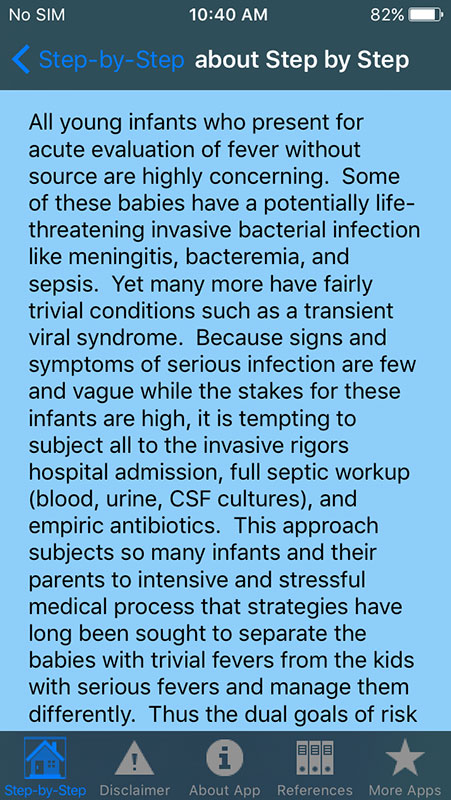
One of the biggest fears that new parents face is the febrile infant. Although being the common clinical problem and one of the main causes for bringing the infants to urgent care, fever also poses a serious challenge to healthcare providers.
The main reason for this is nonspecific symptoms in young febrile infants (ages 0-3 months), which make difficult to distinguish between infants with a viral illness and those with early serious invasive bacterial illness, such as meningitis, sepsis, pneumonia, bacteremia, or urinary tract infection (UTI).
A 2-month old infant with a fever of 102.2 you've just evaluated in the ER can't tell if the risk for invasive bacterial illness is low, intermediate or high. Also, the results of infant evaluation (CRP, neutrophil count, etc.) may indicate both problems.
The fact is that serious bacterial illness is relatively uncommon among febrile infants. Fever is mostly caused by viral infections and is likely to be self-limiting. Still, invasive bacterial illness shouldn't be written off so easily, because if not promptly diagnosed and managed, it may result in serious consequences.
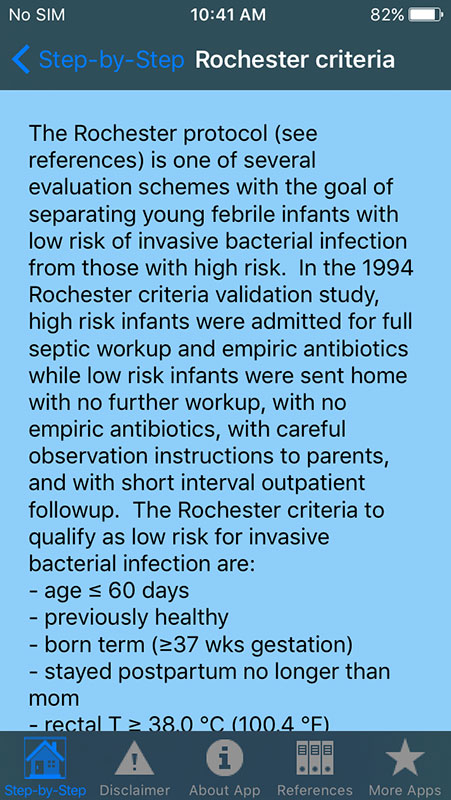
For years, the healthcare providers were using various guidelines using different criteria, such as Rochester criteria, or Lab-Score, in order to determine if the febrile infants are at highest risk of serious bacterial illness. A lot of these guidelines were based on studies written two decades ago when there were no pneumococcal or Hib vaccines available.
Several doctors from Cruces University Hospital in Spain, led by Borja Gomez, MD, recently published a study involving 2,185 infants aged ≤90 days with fever without a source, in which they described a new 'Step-by-Step' approach for identifying febrile infants at risk for invasive bacterial infection[1].
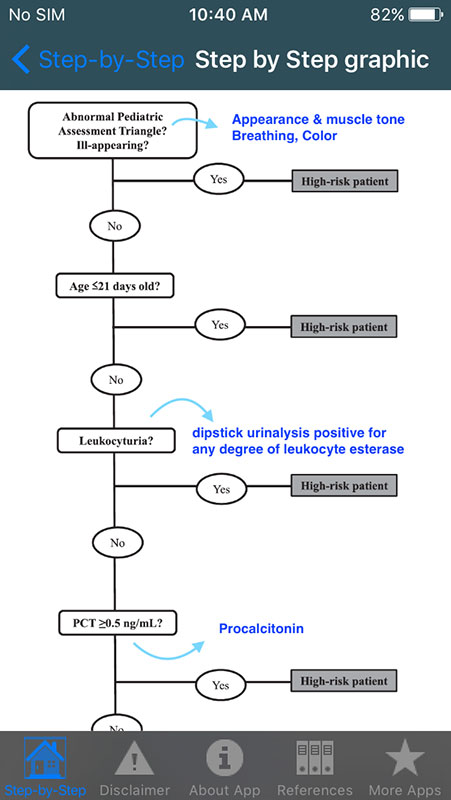
The new approach is based on the algorithm that prioritizes any ill-appearing patient or any patient aged ≤21 days as "high risk." The algorithm then checks if the patient had urinary leukocyturia, checks PCT and CRP levels and neutrophil count, to determine if a patient could be considered a "low-risk" patient and forgo extensive evaluation.
Step-by-Step approach has shown better sensitivity and negative predictive value for ruling out an invasive bacterial illness than Rochester criteria and the Lab-score, the Step-by-Step approach was compared with, in the study. This means it is valid for identifying febrile infants at risk for invasive bacterial infection.
Dr. Joshua Steinberg, a creator of Health Maintenance Visit Checklists app and OB Wheels calendar calculator app we already reviewed, decided to make another useful app based on Step-by-Step approach. With the permission of Dr. Gomez and his colleagues, Dr. Steinberg adapted their validation study and incorporated their evidence-based algorithm into his new app, called Step-by-Step Febrile Infant.
When you start the app, you'll see the note stating that the app was made with the kind permission of study authors. The design of the app is the same as in all other apps made by Dr. Steinberg, i.e. blue background with white grids (options).
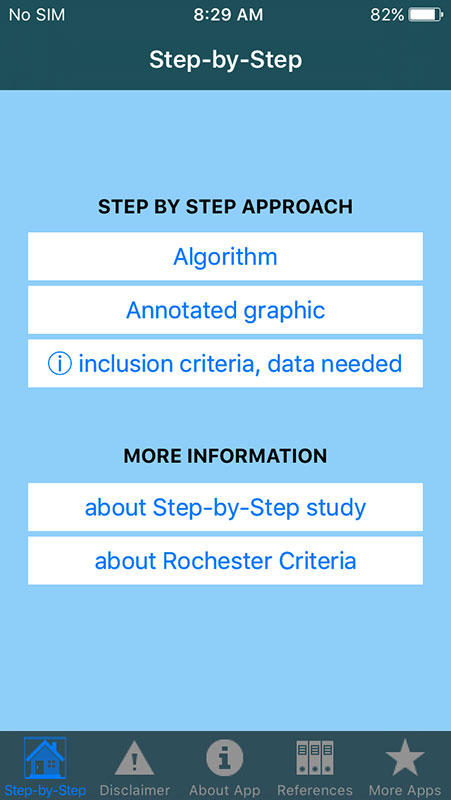
The home screen is simple, allowing you to access the algorithm or to see annotated graphic that explains Step-by-Step approach visually. Also, there is exhaustive information about this approach, as well as about Rochester criteria, as a compared model.
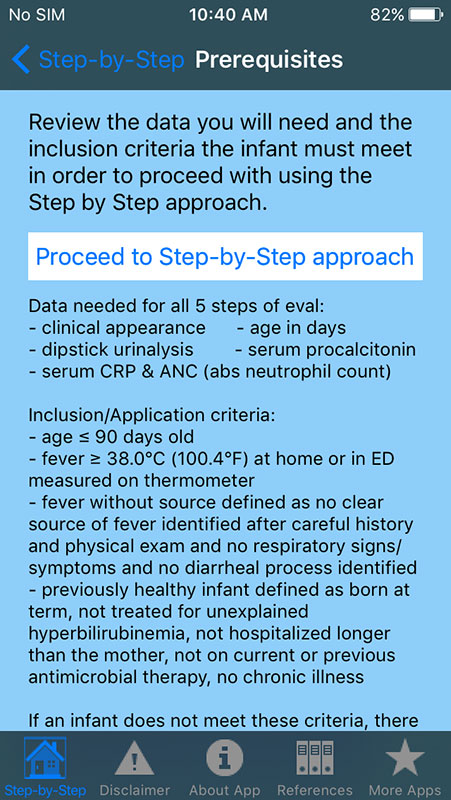
Tapping on algorithm will provide you with brief information about the prerequisites before you can proceed with using the Step-by-Step approach, i.e. data needed for 5 steps of evaluation, and inclusion/application criteria, which infant has to meet in order to be evaluated by this approach. These include the age of the infant (has to be ≤90 days old), fever without a source, which has to be ≥ 100.4°F (38°C), etc.
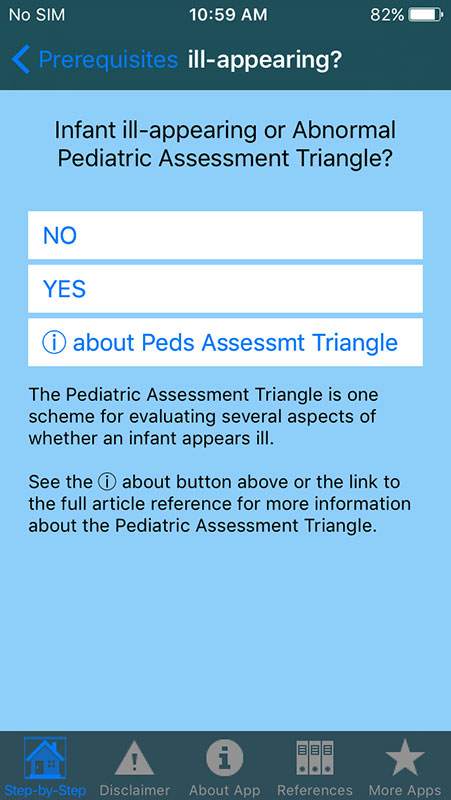
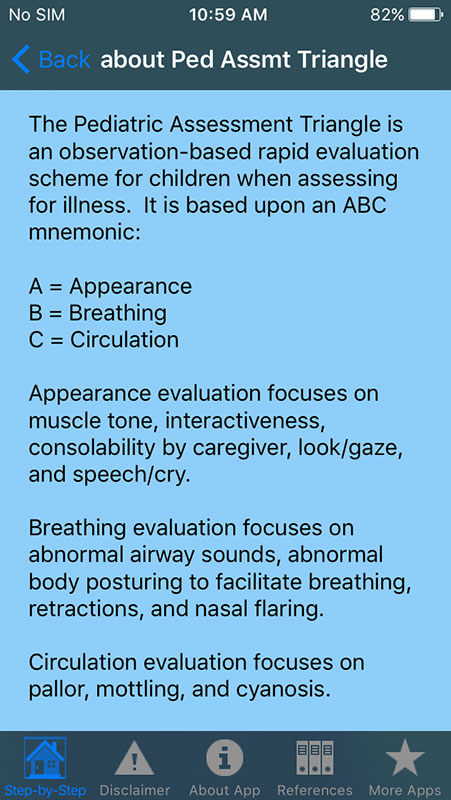
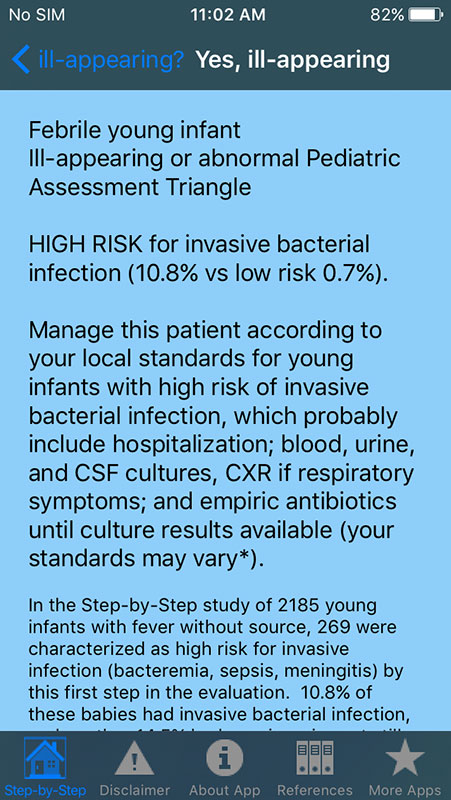
If all prerequisites are met, you may proceed to Step-by-Step approach which will first ask you if the febrile infant is ill-appearing according to Abnormal Pediatric Assessment Triangle. If your answer is yes, the algorithm will suggest that the febrile infant is at high risk of invasive bacterial infection, advising you to manage the patient according to your local standards for infants with high risk of IBI, which most likely include hospitalization.
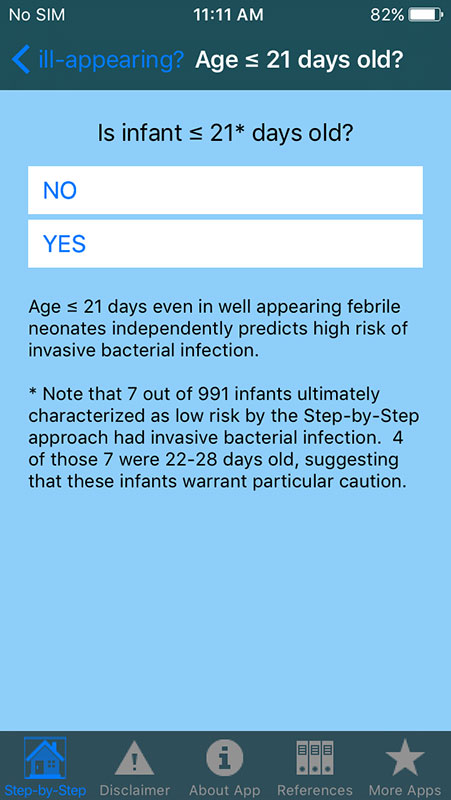
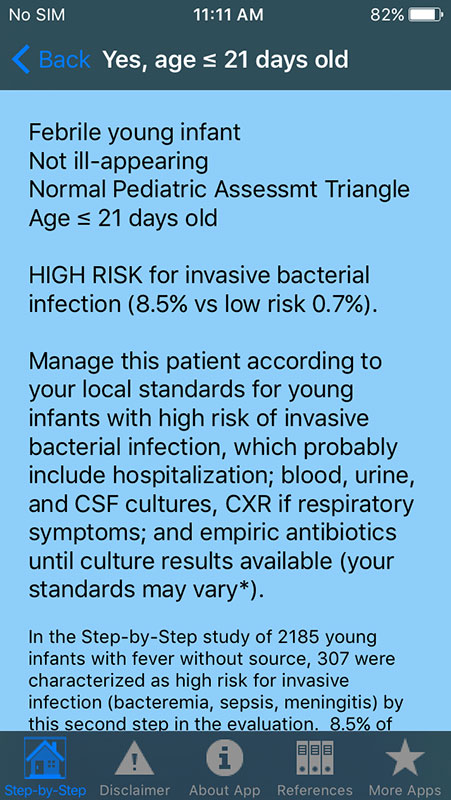
If the answer is no, you'll be asked about the infant's age. If it's ≤21 days old, the algorithm will prioritize the patient as high risk with the same suggestion.
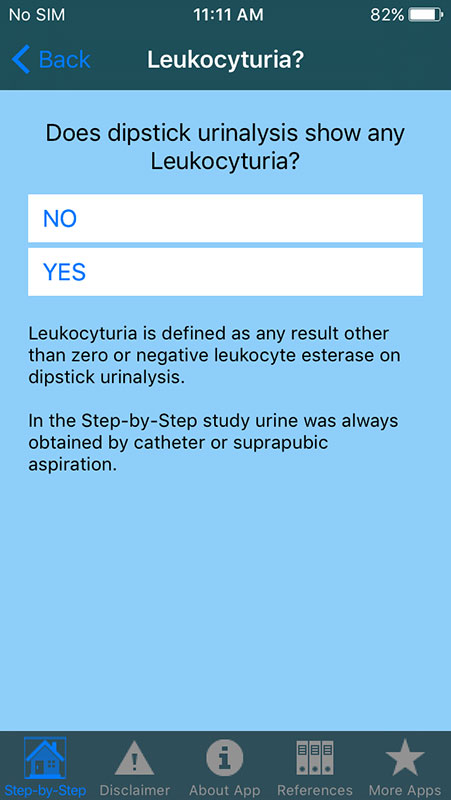
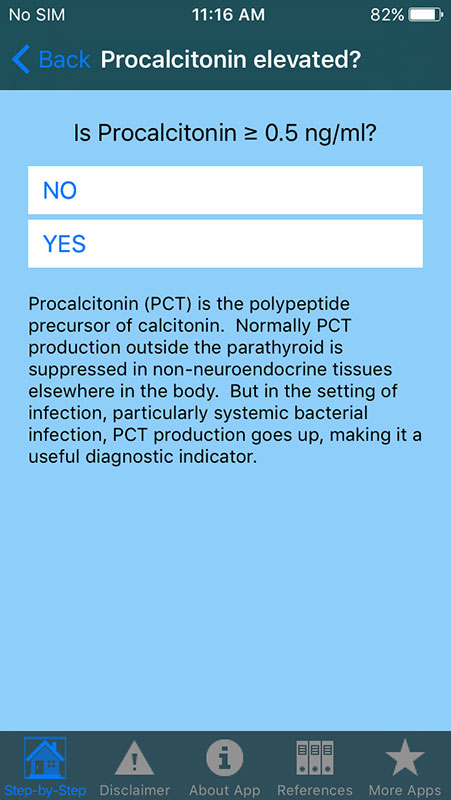
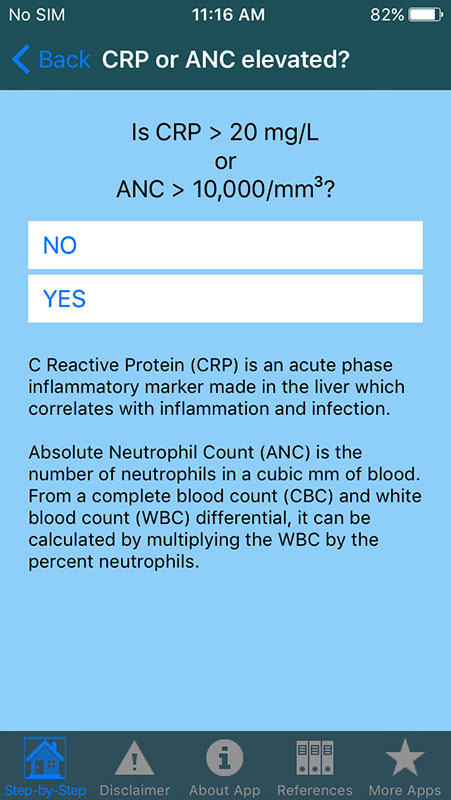
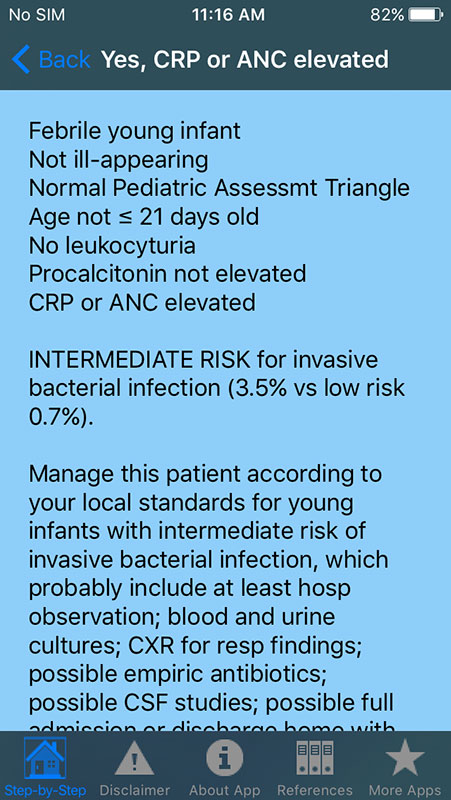
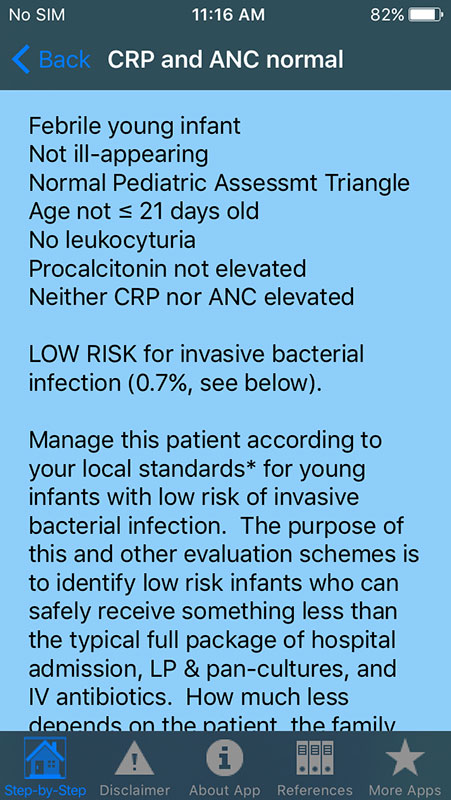
If the infant is older than 21 days, the app will check urinalysis results (if it shows any leukocyturia), followed by the question if Procalcitonin levels are ≥ 0.5 ng/mL, and whether the patient had a CRP level ≥20 µ/L or an absolute neutrophil count > 10,000/mm3.
Any patient failing to meet these criteria is considered a "low-risk" patient with an appropriate suggestion for treatment according to local standards.
The algorithm is quite straightforward and easy-to-use. You basically answer the questions and based on your answers, you get suggestions for further actions.
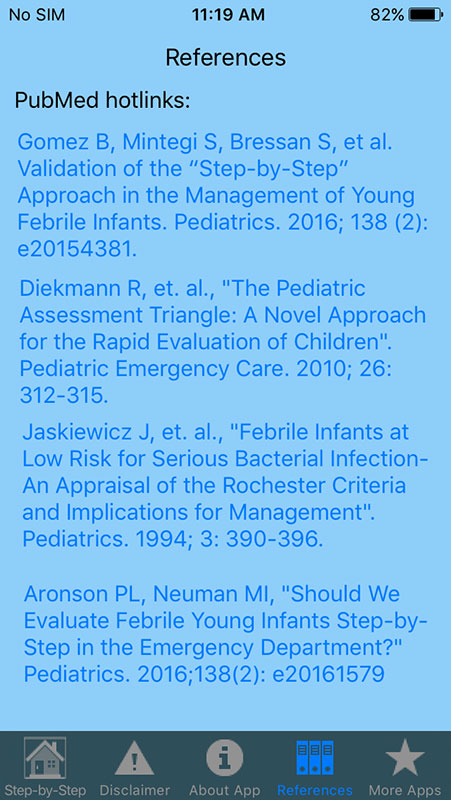
The app is well referenced providing several links, which all lead to PubMed articles, including the study the app is based on, as well as the articles about the Pediatric Assessment Triangle and Rochester Criteria. It, however, omits the information on Lab-score method, which was also used and compared in the reference study.
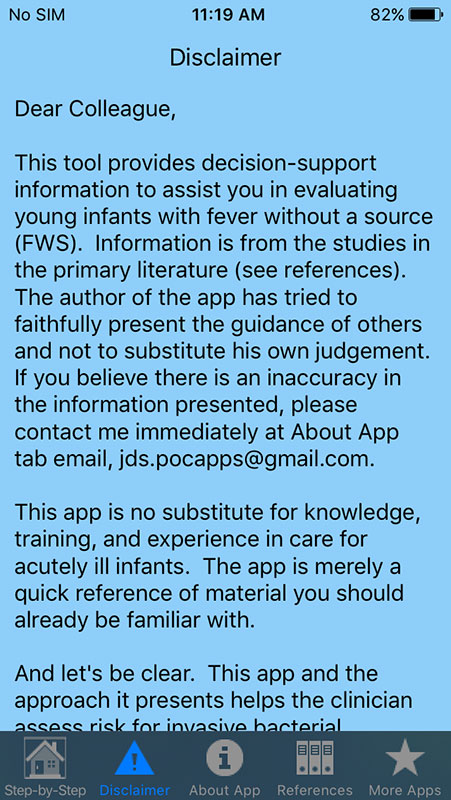
As in any other app made by Dr Joshua Steinberg, there are also sections with a disclaimer, info about the app and links to other apps developed by Dr Steinberg.
Overall, Step-by-Step Febrile Infant is an amazing evidence-based medical app, which uses an improved algorithm to assess the risk of invasive bacterial infection in febrile infants.
Benefit: Any healthcare provider who cares for febrile infants would benefit from this app. The app SHOULD NOT be used by patients and parents.
Verdict:
For- Easy-to-use
- Great evidence-based calculator and decision support tool
- Annotated graph is nice addition
- Well referenced with links to PubMed articles
- Lack of info about Lab-score method
- Not available for Android





























Your thoughts on this
Loading...