Polymyalgia rheumatica is an inflammatory condition that causes devastating pain and stiffness, but it's surprisingly difficult to diagnose. With the right treatment, however, your quality of life can improve drastically and immediately.
Edith, a woman in her 70s, had lived with chronic pain for years — it started with aching shoulders, a pain that soon progressed to her neck, hips, thighs, lower back, and even upper arms. Her mobility declined fast, to the point that she felt stiff when she woke up, couldn't hold a pen to write in her journal any more, and her trouble getting her shoes on. Edith's days became dominated by pain, which didn't subside even with over the counter painkillers.
Then, there was the constant feeling that she was coming down with a flu. Fever, fatigue, weakness, not feeling like eating, and of course the accompanying weight loss. In the end, it got so bad that Edith, one of the elders I care for, couldn't get out of bed at all. She'd just cry, wondering if life was still worth living.
Worst of all? Edith had no idea what was wrong with her. Her doctors could not give her a diagnosis.
What Is Polymyalgia Rheumatica?
A rarely talked-about inflammatory disorder, polymyalgia rheumatica almost always strikes people over 65 years old — and often suddenly, over a period of days or weeks. Once you reach your sixth decade, you often find you already have all kinds of aches and pains, and often also diagnosed or undiagnosed underlying medical conditions. The symptoms of stiffness, pain, and limited movement may be interpreted as being a normal part of the aging process — but they are not.
The stiffness people with polymyalgia rheumatica experience is always worse first thing in the morning, yet the pain they wake up with may cause them to avoid being active and mobile, once again contributing to further stiffness. People with polymyalgia rheumatica will typically experience the following symptoms:
- Stiffness and pain in very varied parts of the body, such as the shoulders, neck, lower back, upper arms, buttocks, thighs, wrists, and ankles.
- Increased stiffness after sleep or after other prolonged periods of physical inactivity.
- A shortened range of motion, including difficulties getting dressed, using tools such as pens or knives, and getting up front a sitting or laying position.
- Sleep difficulties.
- Depression.
- Sometimes fever.
- A feeling of general weakness and malaise.
- A loss of appetite and resultant weight loss.
What Causes Polymyalgia Rheumatica?
Nobody knows, as of yet. But, and you'll have heard this story before, both genetic and environmental factors are thought to be involved in its onset. Though the cause of PMR isn't yet clear, we do know about some definite risk factors. First off, polymyalgia rheumatica is almost always a disease that affects older people, those over 65. It is almost never seen in people under 50. Women and people of North European ethnic origin are also much more likely to develop PMR.
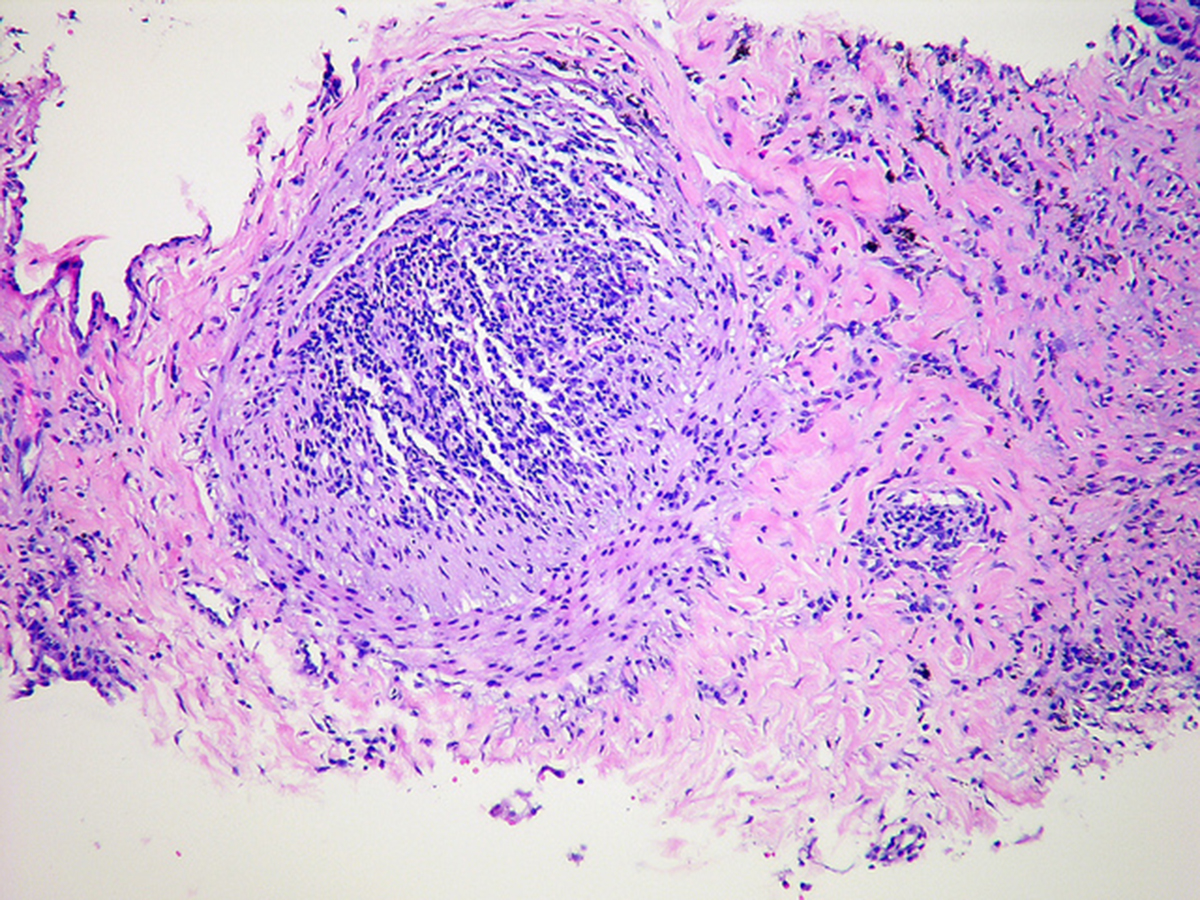
Another thing you need to know about if you suspect you may have polymyalgia rheumatica is that there's another disease that seems to be closely linked to PMR, to the point that some medical professionals believe them to be the same disease. This disease is called giant cell arteritis. One in five PMR patients will show signs of giant cell arteritis, while about half of those diagnosed with giant cell arteritis will have symptoms of PMR. In giant cell arteritis, the arteries become inflammed and patients experience headaches, jaw pain, and vision problems. If left untreated, giant cell arteritis can lead to a stroke and also blindness. Because giant cell arteritis is dangerous, you need to inform your doctor right away if these symptoms sound familiar to you.
Polymyalgia Rheumatica: Diagnosis, Treatment, And A Pain-Free Life
How Do You Know If You Have Polymyalgia Rheumatica?
Causing what looks like generalized symptoms at first sight, polymyalgia is notoriously tricky to diagnose. You are most likely to receive the correct diagnosis if you stumble upon a rheumatologist, who will have been trained to recognize the symptoms of polymyalgia rheumatica, and who will know how they differ from the symptoms of other conditions that appear similar on the surface.
The diagnostic process that serves to determine the cause of your pain and stiffness will start off generally — your healthcare provider will ask you about already known medical conditions, your family background, where in your body you are experiencing your symptoms, when they first arrived, and at which time of the day they are most severe. They will ask you which activities you have difficulty with, and may ask you about your mental health as well.
Polymyalgia rheumatica is a diagnosis of exclusion in many ways. If you have PMR, nonsteroidal anti-inflammatory drugs such as ibuprofen and naproxen will not reduce your pain, while other medications will (we'll get there in a bit). Therefore, your doctor will also ask you how you react to over the counter pain medications, specifically NSAIDs.
Blood tests used to detect inflammation in the body — such as an erythrocyte sedimentation rate test and a C-reactive protein test — can also be employed over the course of the diagnostic process. People with polymyalgia rheumatica will typically show extremely high inflammation rates.
Imaging tests and a physical examination may also be used to determine whether your stiffness is caused by polymyalgia rheumatica, however if your healthcare provider has a very strong incling that you have the disease, they may move straight to prescribing you a low dose of corticosteroids (such as Orasone). Why? If you indeed have polymyalgia rheumatica, you will quickly react to these drugs by showing a remarkable improvement in your symptoms. The very fact that the corticosteroids work for you can confirm the diagnosis of polymyalgia rheumatica. You may get your diagnosis and your "cure" at the same time, in other words.
What Now?
Remember Edith? Once she saw a rheumatologist who suspected she had PMR, things changed for her very rapidly after she was started on corticosteroids. The corticosteroids worked for her, and after years of constant pain, she has now found joy in life again. If your results are anywhere near as good as hers, your "what now?" will simply consist of taking corticosteroids and enjoying your life with a lot less pain and a lot more mobility. Because corticosteroids can have side effects, even unpleasant ones like osteoporosis, cataracts, thinner skin and high blood sugar levels, you will, however, need to see your doctor for regular checkups from this point forward. You will also need to watch out for signs of giant cell arteritis.



Your thoughts on this