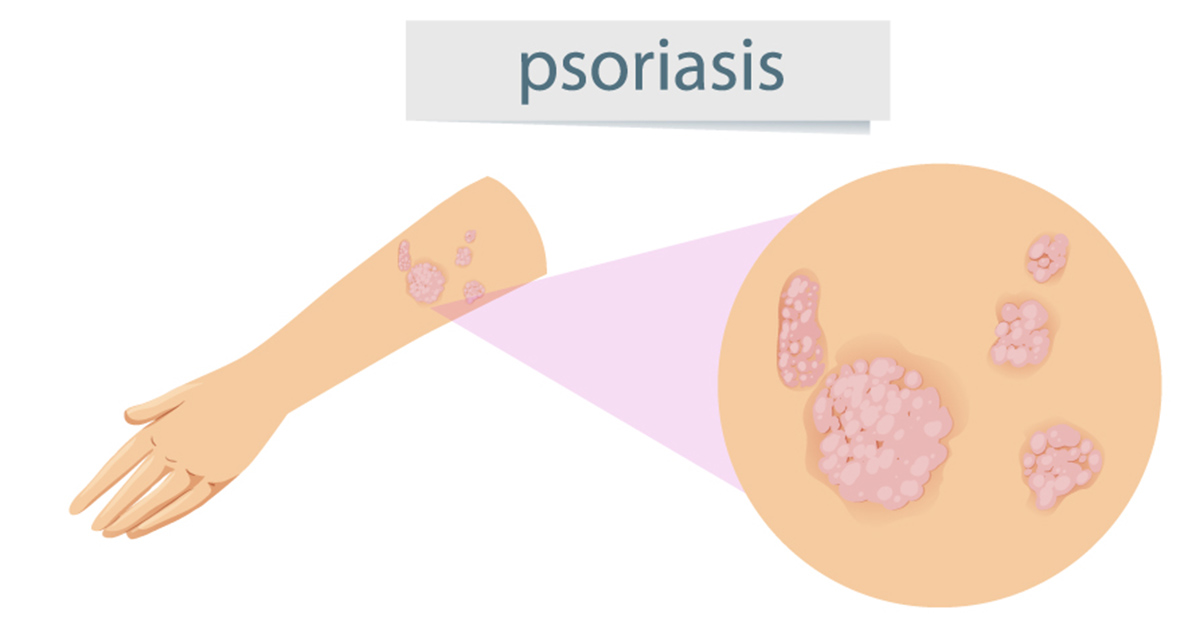
There are more than a 100 different types of arthritis, including a subtype known as psoriatic arthritis. Generally, psoriatic arthritis develops in patients that have a skin condition called psoriasis, which is a disease that is associated with a red, scaly skin rash that frequently develops in the hands, elbows, ankles, feet, knees, and other areas. Patients with psoriatic arthritis develop inflamed and swollen joints that become stiff and painful.
Studies estimate that up to two in every five people who have psoriasis will eventually go on to develop psoriatic arthritis. If it develops, psoriatic arthritis will generally manifest within 10 years of receiving a diagnosis of psoriasis. In a subset of patients, the symptoms associated with psoriatic arthritis actually manifest before any symptoms of psoriasis.
Similar to psoriasis, psoriatic arthritis is a chronic condition that progressively worsens. Furthermore, in patients with severe psoriatic arthritis, there is high risk that that their joints will become permanently damaged and require surgery down the road.
It is important to recognize and diagnose psoriatic arthritis early on as early intervention can help slow down the progression of the disease and minimize any permanent damage to the joints.
Causes of psoriatic arthritis
Similar to the cause of psoriasis and several other types of arthritis, researchers believe that psoriatic arthritis develops as a result of autoimmunity. Generally, the immune system is present in our body to protect us from other, foreign pathogens. However, in the case of an autoimmune disease, the immune system becomes impaired and starts to attack our own healthy tissue, leading to the development of disease and symptoms.
At this point, researchers are not sure why some people with psoriasis develop psoriatic arthritis while other people don’t. These are the factors that can trigger the development of psoriasis:
- Injury to the skin
- Sunlight
- Infections, such as streptococcal infections and HIV
- Drugs including lithium, beta-blockers and anti-malarials
- Emotional stress
- Smoking
- Alcohol
- Hormonal changes
Symptoms of psoriatic arthritis
Symptoms can vary from person to person and the severity of symptoms also tends to vary. While some people will experience symptoms that affect multiple joints, others will only have mild symptoms in one or two joints.
The symptoms that affect patients with psoriatic arthritis are:
- Pain, swelling and stiffness of any joint in the body, particularly the knees, neck, hands, feet, spine and elbows.
- Fatigue or weakness.
- Swollen fingers or toes.
- Red, itchy and scaly skin.
- Thick, gray scaly areas on the skin.
- Inflammation of the eye.
Symptoms tend of psoriatic arthritis tend to often be cyclical. They get worse during periods known as flare-ups or relapses and improve during periods known as remission. Unfortunately, it is difficult to predict when a relapse will occur, but it can be managed with the right medication.
Diagnosis: How is psoriatic arthritis diagnosed?
If your physician suspects that you may have psoriatic arthritis, they will likely refer you to a specialist called a rheumatologist. The rheumatologist will take into account a number of different factors when trying to figure out a diagnosis including symptoms, medical and personal history, physical exam, the presence of psoriasis and other tests. These are the tests that the doctor may order:
- Blood tests that look for erythrocyte sedimentation rate (which point to levels of inflammation in the body) and rheumatoid factor (which helps exclude a diagnosis of rheumatoid arthritis).
- Genetic tests. More than 50 percent of people with psoriatic arthritis that have spine inflammation have a gene called HLA-B27. The doctor may order a genetic test to see if you carry the gene.
- Imaging tests such as X-rays can show joint damage or any changes to cartilage that have occurred. These changes in the spine, hands, or feet can suggest a diagnosis of arthritis. People that have psoriatic arthritis tend to have different X-ray findings than people with rheumatoid arthritis.
- Bone density tests. Psoriatic arthritis can lead to bone loss so the doctor may order bone density tests to see if you have bone loss.
Treatments: How is psoriatic arthritis managed?
Currently, there is no cure for psoriatic arthritis. However, there are treatments that can help manage the condition by relieving symptoms, slowing down progression of the disease and improving patients' quality of life.
Most people end up taking multiple medications to manage their symptoms, some of which can also treat the underlying psoriasis. However, it is ideal to only take one type of medication for both the conditions. These are the different types of medications that the doctor may prescribe:
- Non-steroidal anti-inflammatory drugs (NSAIDs). Doctors can prescribe two different types of NSAIDs: traditional NSAIDs (such as ibuprofen) or COX-2 inhibitors (such as celecoxib). NSAIDs help reduce inflammation and pain. Some side effects include indigestion and stomach ulcers.
- Corticosteroids. Similar to NSAIDs, corticosteroids reduce pain and swelling. Corticosteroids are often administered as an injection straight into a single inflamed or swollen joint, with the effect lasting from weeks to months. They can also be taken as a tablet. It is important to note that corticosteroids carry significant side effects when used in the long-term.
- Disease-modifying anti-rheumatic drugs (DMARDs). DMARDs, such as leflunomide, work by addressing the underlying condition. Use of DMARDs is associated with an ease of symptoms and slowdown in the progression of the disease. DMARDs can take anywhere from several weeks to months to work.
- Biological therapies. Biological therapies are a new type of treatment for psoriatic arthritis and can be administered a patient doesn’t respond to DMARDs. Biological therapies work by reducing levels of chemicals in the body that cause inflammation. A common biological therapy is adalimumab, which blocks TNF (an inflammatory molecule in the blood). There can be several side effects associated with the use of biological therapies including higher chance of developing infections, problems with liver or kidney, and several others.
- Gladman, D. D., et al. "Psoriatic arthritis: epidemiology, clinical features, course, and outcome." Annals of the rheumatic diseases 64.suppl 2 (2005): ii14-ii17.
- Taylor, William, et al. "Classification criteria for psoriatic arthritis: development of new criteria from a large international study." Arthritis & Rheumatism: Official Journal of the American College of Rheumatology 54.8 (2006): 2665-2673.
- Ritchlin, Christopher T., et al. "Treatment recommendations for psoriatic arthritis." Annals of the rheumatic diseases 68.9 (2009): 1387-1394.
- Photo courtesy of SteadyHealth.com


Your thoughts on this