Overview
The clots that form during this condition can lodge in other small vessels and cause damage to organs such as the brain, heart, and kidneys.
Causes
TTP occurs as a result of the spontaneous aggregation of platelets in the bloodstream and this is caused by a variety of factors. These include the following processes:
- Autoimmune reaction - inhibition of the enzyme ADAMTS13 by antibodies produced by the body's immune system has been hypothesized to result in increased levels of von Willebrand factor (vWF). When vWF isn't broken down by the ADAMTS13 enzyme, this results in an increased chance of blood clots forming in the bloodstream.
- Congenital - in this case, the process of TTP occurs the same as it does in the autoimmune subtype but the problem lies in a mutation of the ADAMTS13 enzyme rather than it being inactivated by antibodies.
- Secondary causes - 40 percent of all cases of TTP have a secondary cause to them. Predisposing factors to this condition may include pregnancy, certain cancers, bone marrow transplantation, using medications such as quetiapine, quinine, chemotherapeutic medications, bone marrow transplantation, immunosuppressants, and drugs that alter hormone levels, and infection with HIV.
Symptoms and Signs
The symptoms and signs of TTP may be non-specific since there are other conditions that can mimic the clinical presentation of this disease.
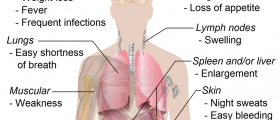
Many affected patients may experience issues such as flu-like symptoms before developing TTP. Common issues that may occur include generalized fatigue, headaches, and confusion.
As the condition progresses, bruising and rarely bleeding may occur as a result of decreased platelet levels. The bruising takes on the form of purpura and even larger marks known as ecchymoses. If bleeding occurs, then it will commonly involve the gums or the nose.
The classical presentation of TTP though involves the combination of five specific medical signs and they include:
- Changes in the patient's mental status.
- Fever.
- Decreased function of the kidneys.
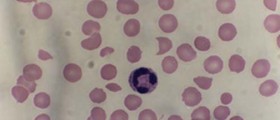
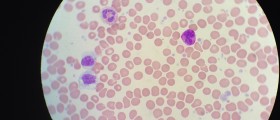
- Reduced platelet levels in the bloodstream.
- Hemolytic anaemia where the red blood cells rupture.
Management
Other medications are given concomitantly with plasmapheresis such as corticosteroids to help reduce the inflammatory process that occurs in TTP.
In cases where TTP fails to respond to plasmapheresis and corticosteroids, the monoclonal antibody rituximab is used to kill the B cells in the bloodstream and this helps to reduce the inhibitor of the ADAMTS13 enzyme.
Patients who develop relapsing or refractory TTP receive additional immunosuppressant medications such as cyclophosphamide and vincristine. If these medications are also deemed ineffective, then surgical intervention through the performance of a splenectomy (removal of the spleen) may be considered.
Prognosis
In untreated cases, the mortality rate of patients with TTP is 95 percent.
- www.ncbi.nlm.nih.gov/pmc/articles/PMC3159000/
- Photo courtesy of SteadyHealth