Is there any conection between ITP and von willibrands disease? could somebody be diagnosed with ITP when really they have von willibrands?
Loading...
There is no connection between ITP and von Willebrand disease. It is possible, however, to misdiagnose ITP for von Willebrand or visa versa since their presentation can be similar.
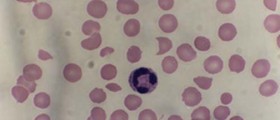
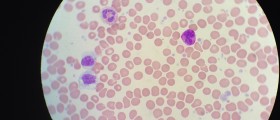
Idiopathic thrombocytopenic purpura (ITP) is the condition of having a low platelet count (thrombocytopenia) of no known cause (idiopathic). As most causes appear to be related to antibodies against platelets, it is also known as immune thrombocytopenic purpura or immune-mediated thrombocytopenic purpura. Although most cases are asymptomatic, very low platelet counts can lead to bleeding diathesis and purpura.
Von Willebrand disease (vWD) is the most common hereditary coagulation abnormality described in humans, although it can also be acquired as a result of other medical conditions. It arises from a qualitative or quantitative deficiency of von Willebrand factor (vWF), a multimeric protein that is required for platelet adhesion.
So, both are coagulation abnormalities that present with varying degrees of bleeding tendency.
They can be distinguished with lab tests.
ITP
The diagnosis of ITP is a process of exclusion. First, the clinician has to determine that there are no blood abnormalities other than low platelet count, and no physical signs except for signs of bleeding. Then, the secondary causes (usually 5–10 percent of suspected ITP cases) should be excluded. Secondary causes could be leukemia, medications (e.g. quinine, heparin), lupus erythematosus, cirrhosis, HIV, hepatitis C, congenital causes, antiphospholipid syndrome, von Willebrand factor deficiency and others. In approximately one percent of cases, autoimmune hemolytic anemia and immune thrombocytic purpura coexist, which is a condition called Evans syndrome.
Despite the destruction of platelets by splenic macrophages, the spleen is normally not enlarged. In fact, an enlarged spleen should lead a clinician to investigate other possible causes for the thrombocytopenia.
Bleeding time is prolonged in ITP patients. However, the use of bleeding time in diagnosis is discouraged by the American Society of Hematology practice guidelines. A normal bleeding time does not exclude a platelet disorder.
A bone marrow examination may be performed on patients over the age of 60 and those who do not respond to treatment, or when the diagnosis is in doubt. On examination of the bone marrow, an increase in the production of megakaryocytes is seen and can help in determining if it's ITP. The blood analysis for the antiplatelet antibodies is a matter of clinician's preference, as there is a disagreement whether the 80 percent specificity of this test is sufficient.
von Willebrand
When von Willebrand is suspected, blood plasma of a patient needs to be investigated for quantitative and qualitative deficiencies of vWF. This is achieved by measuring the amount of vWF in a vWF antigen assay and the functionality of vWF with a glycoprotein (GP)Ib binding assay, a collagen binding assay or, a ristocetin cofactor activity (RiCof) or ristocetin induced platelet agglutination (RIPA) assays. Factor VIII levels are also performed as factor VIII is bound to vWF which protects the factor VIII from rapid breakdown within the blood. Deficiency of vWF can therefore lead to a reduction in factor VIII levels. Normal levels do not exclude all forms of vWD: particularly type 2 which may only be revealed by investigating platelet interaction with subendothelium under flow (PAF), a highly specialized coagulation study not routinely performed in most medical laboratories. A platelet aggregation assay will show an abnormal response to ristocetin with normal responses to the other agonists used. A platelet function assay (PFA) will give an abnormal collagen/adrenaline closure time and in most cases (but not all) a normal collagen/ADP time. Type 2N can only be diagnosed by performing a "factor VIII binding" assay. Detection of vWD is complicated by vWF being an acute phase reactant with levels rising in infection, pregnancy and stress.
Other tests performed in any patient with bleeding problems are a complete blood count (especially platelet counts), APTT (activated partial thromboplastin time), prothrombin time, thrombin time and fibrinogen level. Testing for factor IX may also be performed if hemophilia B is suspected. Other coagulation factor assays may be performed depending on the results of a coagulation screen. Patients with Von Willebrand disease will typically display a normal prothrombin time and a variable prolongation of partial thromboplastin time.
Idiopathic thrombocytopenic purpura (ITP) is the condition of having a low platelet count (thrombocytopenia) of no known cause (idiopathic). As most causes appear to be related to antibodies against platelets, it is also known as immune thrombocytopenic purpura or immune-mediated thrombocytopenic purpura. Although most cases are asymptomatic, very low platelet counts can lead to bleeding diathesis and purpura.
Von Willebrand disease (vWD) is the most common hereditary coagulation abnormality described in humans, although it can also be acquired as a result of other medical conditions. It arises from a qualitative or quantitative deficiency of von Willebrand factor (vWF), a multimeric protein that is required for platelet adhesion.
So, both are coagulation abnormalities that present with varying degrees of bleeding tendency.
They can be distinguished with lab tests.
ITP
The diagnosis of ITP is a process of exclusion. First, the clinician has to determine that there are no blood abnormalities other than low platelet count, and no physical signs except for signs of bleeding. Then, the secondary causes (usually 5–10 percent of suspected ITP cases) should be excluded. Secondary causes could be leukemia, medications (e.g. quinine, heparin), lupus erythematosus, cirrhosis, HIV, hepatitis C, congenital causes, antiphospholipid syndrome, von Willebrand factor deficiency and others. In approximately one percent of cases, autoimmune hemolytic anemia and immune thrombocytic purpura coexist, which is a condition called Evans syndrome.
Despite the destruction of platelets by splenic macrophages, the spleen is normally not enlarged. In fact, an enlarged spleen should lead a clinician to investigate other possible causes for the thrombocytopenia.
Bleeding time is prolonged in ITP patients. However, the use of bleeding time in diagnosis is discouraged by the American Society of Hematology practice guidelines. A normal bleeding time does not exclude a platelet disorder.
A bone marrow examination may be performed on patients over the age of 60 and those who do not respond to treatment, or when the diagnosis is in doubt. On examination of the bone marrow, an increase in the production of megakaryocytes is seen and can help in determining if it's ITP. The blood analysis for the antiplatelet antibodies is a matter of clinician's preference, as there is a disagreement whether the 80 percent specificity of this test is sufficient.
von Willebrand
When von Willebrand is suspected, blood plasma of a patient needs to be investigated for quantitative and qualitative deficiencies of vWF. This is achieved by measuring the amount of vWF in a vWF antigen assay and the functionality of vWF with a glycoprotein (GP)Ib binding assay, a collagen binding assay or, a ristocetin cofactor activity (RiCof) or ristocetin induced platelet agglutination (RIPA) assays. Factor VIII levels are also performed as factor VIII is bound to vWF which protects the factor VIII from rapid breakdown within the blood. Deficiency of vWF can therefore lead to a reduction in factor VIII levels. Normal levels do not exclude all forms of vWD: particularly type 2 which may only be revealed by investigating platelet interaction with subendothelium under flow (PAF), a highly specialized coagulation study not routinely performed in most medical laboratories. A platelet aggregation assay will show an abnormal response to ristocetin with normal responses to the other agonists used. A platelet function assay (PFA) will give an abnormal collagen/adrenaline closure time and in most cases (but not all) a normal collagen/ADP time. Type 2N can only be diagnosed by performing a "factor VIII binding" assay. Detection of vWD is complicated by vWF being an acute phase reactant with levels rising in infection, pregnancy and stress.
Other tests performed in any patient with bleeding problems are a complete blood count (especially platelet counts), APTT (activated partial thromboplastin time), prothrombin time, thrombin time and fibrinogen level. Testing for factor IX may also be performed if hemophilia B is suspected. Other coagulation factor assays may be performed depending on the results of a coagulation screen. Patients with Von Willebrand disease will typically display a normal prothrombin time and a variable prolongation of partial thromboplastin time.
Loading...