I was recently reading a lot about 48,XXYY Syndrome, which can strike boys only. From what I read, there is a definite connection between 48,XXYY Syndrome and gynaecomastia, in adolescents. Is this true? Why is that the case? Is there anything that we can do to prevent this from happening to any individual patient with 48,XXYY Syndrome?
Loading...
Hi, I'm on the advisory board for the XXYY Project (an organization that supports families of boys with 48XXYY), and I consulted with our medical director Dr. Nicole Tartaglia - who gives the following answer:
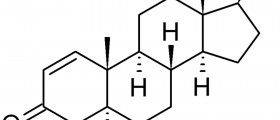
There is an increased risk of gynecomastia in adolescent and adult males with XXYY, and in any condition in which a male has one or more extra X chromosomes including XXY (Klinefelter syndrome), XXXY and XXXXY. Gynecomastia is defined as growth of the breast tissue in males, and it is seen in about 10-20% of all males (typical XY males included) during early puberty. In most XY males, the gynecomastia resolves within 1-2 years. In all males, the appearance of “breasts” increases in males who have more adipose tissue (fat tissue), so it is important to differentiate between gynecomastia and adipose tissue. For a true diagnosis of gynecomastia, there must be palpable breast tissue beneath the adipose tissue. In XXYY, the gynecomastia may remain after puberty, and about 25% of adolescent and adult males with XXYY have gynecomastia. In most cases, the finding is mild and not usually evident in clothing. In adolescents with XXYY, the testicles usually do not make sufficient testosterone to support complete pubertal development, and testosterone replacement treatment is needed. It is believed that gynecomastia may be prevented by initiating testosterone replacement therapy when it starts to become deficient in XXYY. However, even with appropriate testosterone therapy there are still some cases of XXYY syndrome with gynecomastia. If it persists and the individual with XXYY is self-conscious about it, the tissue can be removed surgically through a straightforward surgical procedure.
**********************************************************************
Nicole Tartaglia, MD
Assistant Professor, Department of Pediatrics
University of Colorado at Denver, School of Medicine
Developmental-Behavioral Pediatrics
Child Development Unit, The Children's Hospital
13123 East 16th Ave, B140
Aurora, CO 80045
There is an increased risk of gynecomastia in adolescent and adult males with XXYY, and in any condition in which a male has one or more extra X chromosomes including XXY (Klinefelter syndrome), XXXY and XXXXY. Gynecomastia is defined as growth of the breast tissue in males, and it is seen in about 10-20% of all males (typical XY males included) during early puberty. In most XY males, the gynecomastia resolves within 1-2 years. In all males, the appearance of “breasts” increases in males who have more adipose tissue (fat tissue), so it is important to differentiate between gynecomastia and adipose tissue. For a true diagnosis of gynecomastia, there must be palpable breast tissue beneath the adipose tissue. In XXYY, the gynecomastia may remain after puberty, and about 25% of adolescent and adult males with XXYY have gynecomastia. In most cases, the finding is mild and not usually evident in clothing. In adolescents with XXYY, the testicles usually do not make sufficient testosterone to support complete pubertal development, and testosterone replacement treatment is needed. It is believed that gynecomastia may be prevented by initiating testosterone replacement therapy when it starts to become deficient in XXYY. However, even with appropriate testosterone therapy there are still some cases of XXYY syndrome with gynecomastia. If it persists and the individual with XXYY is self-conscious about it, the tissue can be removed surgically through a straightforward surgical procedure.
**********************************************************************
Nicole Tartaglia, MD
Assistant Professor, Department of Pediatrics
University of Colorado at Denver, School of Medicine
Developmental-Behavioral Pediatrics
Child Development Unit, The Children's Hospital
13123 East 16th Ave, B140
Aurora, CO 80045
Loading...