The AIDS crisis in Africa seemed to be abating, but in the last year or two it seems to be once again spiraling out of control. The response of public health officials in Africa, however, presents some good ideas for "poz" people all over the world.
Just How Bad Is the HIV Crisis in Africa?
The Republic of South Africa keeps reliable statistics on the numbers of its HIV-positive citizens. In South Africa, the number of people aged 10 to 19 who have HIV has increased 1600 percent over the last 10 years, to approximately 237,000. A very few of these infectees caught the virus during sex. Most were infected at birth. New prophlyactic measures make mother-to-child transmission relatively rare, but they were not available when these South Africans were born. HIV rates in newborns and in children under the age of five are going down, but in teenagers, not only are many more teens dealing with the disease, more of them are not getting treatment that keeps the disease under control. Among 10- to 14-year-olds, about 69 percent are not progressing to AIDS. Among 15- to 19-year-olds, only about 62 percent are not progressing from HIV+ status to full-blown AIDS, according to Mhairi Maskew, Senior Researcher at Health Economics and Epidemiology Research Office in Cape Town.
Other countries in sub-Saharan Africa fail to keep reliable statistics but probably are experiencing the same trends.
What Is Being Done About the Teen HIV Crisis in Africa?
Unlike many states in the United States, the government of South Africa does not have any expectation that teens won't have sex, even if they have HIV. Neither is the government counting on teens to buy and use condoms before they have intercourse. Instead, public health officials are encouraging teens to use a medication called PrEP.
What is PrEP?
In the United States, this drug is known as Truvada. It's a combination of two antiviral drugs that, if taken just before and for two days after sexual intercourse greatly reduces (but doesn't completely eliminate) the chances of getting an HIV infection. Studies of use of the drug by gay men in California suggest that it reduces the risk of transmission on average about 86 percent. In the United States, Truvada is a medication that is taken every day, but in South Africa, PrEP is an "on demand" drug, only taken when one has sexual intercourse or in anticipation of having sexual intercourse right away.
READ Early Start Of HIV Treatment Benefits Patients' Long-Term Health
The South government has found that about 75 percent of HIV+ teens are willing to take the drug. Critics complain that the medication encourages promiscuity and discourages the use of condoms, which would stop or reduce the transmission of other sexually transmitted diseases and prevent pregnancy. In the United States, ironically, surveys find that users of Truvada are more likely to use condoms because taking the drug reminds them of their vulnerability to AIDS. In South Africa, however, arguments against the use of the medication are also made on grounds of morality.
What Can Teens Everywhere Do to Prevent Getting HIV?
American health officials are sometimes forced by law to advocate for abstinence rather than to encourage HIV-positive teens to use drugs like Truvada in combination with condoms when they have sex. Insurance companies are reticent to pay for the drug, which can cost as much as $1,540 for a month's supply when purchased retail. (The Gilead Advancing Access Program can help people who don't have insurance or whose insurance won't pay for the medication; if approved for the program, the company may help with up to $3,600 of drug cost per year. This would be enough for an on-demand schedule for users who do not have sex more often than about once every 10 days.) However, not everyone can take Truvada because of its side effects.
Your best bets for avoiding HIV if you can't take the prophylactic drug are:
- Avoid especially risky sex. Any kind of rough sex that induces bleeding, sex with hard sex toys, sex despite symptoms of herpes or other viral infections (which make it easier for HIV to overpower the immune system), sex with strangers, sex with multiple partners, sex with paid sex workers, and sex in a setting where there is IV drug use are far more likely to result in HIV transmission.
- Avoid exchange of fluids. "On me not in me" is the usual recommendation of HIV experts. Masturbation is less risky than intercourse. Oral intercourse is less risk than vaginal intercourse. Vaginal intercourse is less risky than anal intercourse. However, any kind of intercourse can transmit the virus.
- Don't indulge in anonymous sex. Call the morning after, and the next week, too. HIV transmission often causes flu-like symptoms in its very earliest stages, before the virus is detectable with blood tests. After these initial symptoms pass, there aren't usually any more obvious symptoms for months or years, sometimes up to five years. If your partner gets these symptoms, and you don't know your own HIV status, it's a good idea to get tested.
- If you choose to have sex with an HIV-positive person, he or she should be on drugs to suppress the virus. Even unprotected sex is a lot less risky when the infected partner is on antiviral medications.
- Guys who get circumcisions as teenagers should avoid sexual intercourse until the cut is fully healed. Broken skin around the head of the penis is extremely susceptible to viral infections.
- Avoid club drugs, such as cocaine/crack, crystal methamphetamine, amphetamines, ketamine, methylenedioxymethamphetamine (MDMA/ecstasy), and gamma hydroxybutyric acid (GHB). People taking those drugs tend to engage in sexual behaviors they can only tolerate when they are using the recreational drug. Gay males may use them so they can tolerate receiving anal intercourse. There are more incidents of sex without a condom and sex that breaks a condom when these drugs are part of sex.
READ Sixty-Second HIV Testing Now Available In The USA
Sex can be a beautiful experience, and the more romantic, considerate, and clean sexual relationships are, the safer they are for the teens who experience them. Even if you can't wait to have sex, at least wait long enough to do sex well, as a loving act that won't endanger the health of the person with whom you are intimate.
- Britta L. Jewell, Ide Cremin, Michael Pickles, Connie Celum, Jared M. Baeten, Sinead Delany-Moretlwe, Timothy B. Hallett. Estimating the Cost-Effectiveness of Pre-Exposure Prophylaxis to Reduce HIV-1 and HSV-2 Incidence in HIV-Serodiscordant Couples in South Africa. PLoS One. 2015. 10(1): e0115511. Published online 2015 January 23. doi: 10.1371/journal.pone.0115511 PMCID: PMC4304839.
- Photo courtesy of london: www.flickr.com/photos/london/75148497/
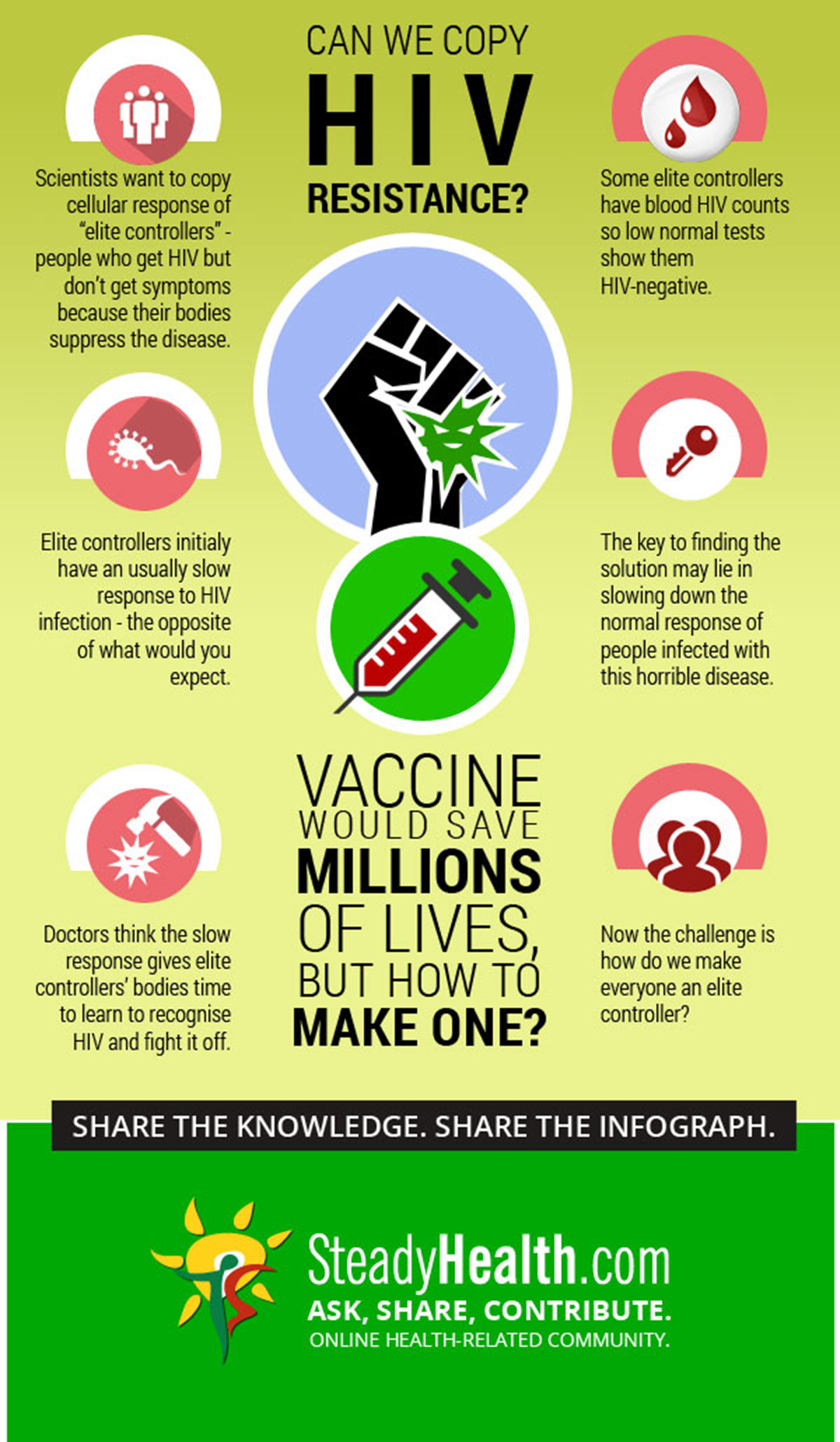
- Infographic by SteadyHealth.com
- Infographic by SteadyHealth.com


Your thoughts on this