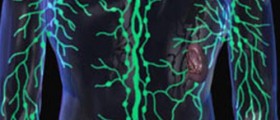
Lymphedema is a common complication of a legion of health conditions. In the developing world, it is not unusual to see grotesquely enlarged arms and legs infected with a parasite that causes a condition called filiriasis, spread by mosquitoes. In industrialized nations, lymphedema is a common complication of surgery for cancer in which lymph nodes are removed to stop the spread of the malignancy. Morbid obesity can cause lymphedema, as can congestive heart failure, vascular surgery, cellulitis and other tunneling skin infections, burns and burn scar treatment, insect bites, poorly planned liposuction or lipectomy, portal hypertension, insect bites, and traumatic injury. Lymphedema can also be idiopathic, appearing on its own, sometimes caused by genetic conditions that also cause yellow nail syndrome, Klinefelter's syndrome, Noonan syndrome, Turner syndrome, trisomy 13, trisomy 18, and trisomy 21.

In every case, however, lymphedema causes persistent swelling as protein-filled fluid accumulates under the skin. At first the two arms or the two legs may simply seem assymetrical. Then swelling becomes obvious. In addition to swelling, there can be gradually increasing immobility. As the leg or arm grows larger, it becomes harder to lift or move. The skin can become tight that it fissures, the breaks in the skin inviting infection. Usually lymphedema occurs in the feet and lower legs, but it can also occur in the arms, trunk, genitals, and face.
There are some very basic things anyone can do to minimize the effects of lymphedema, no doctor's prescription required:
- For lymphedema affecting the lower legs and feet, elevation is important The rule is "nose above toes." Elevating the leg at night helps fluid drain. Just prop up the affected foot or leg on two or three pillows, using just one under the head. It is not necessary to keep the leg elevated during the day.
- Almost any location on the body affected by lymphedema can benefit for compression bindings. Bindings that don't offer at least 40 mm Hg pressure (enough pressure to raise Hg in a blood pressure meter 40 mm, the manufacturer will measure this for you) won't do the job. Either compression stockings (no prescription required, although getting insurance to pay for them requires a doctor's prescription) or a compression pump will do the job. Any kind of compression binding must be comfortable, and there should never be any kind of tourniquet effect. Using a compression pump as soon as the lymphedema is noticed (that is, within days, not months) will prevent the formation of fibrous tissue that makes the swelling permanent.
- Manual lymphatic drainage, pressing on areas of fluid accumulation to move the fluid toward the heart (pressing the wrong direction makes the problem worse) nearly always helps. Regular manual drainage helps the body build collateral blood vessels, which carry fluid away from the swelling. Usually it takes 30 to 35 treatments for collateral blood vessel growth to begin. Treatment every day (or five days a week) is optimal. Interestingly, one study found that manual lymphatic drainage also improved IQ scores.
- Massage therapy relieves swelling for a day or two.
- Exercise helps lymphatic fluid drain if the swollen region is properly supported. You don't want an injury to complicate recovery even more.
- Miaskowski C, Dodd M, Paul SM, West C, Hamolsky D, Abrams G, et al. Lymphatic and Angiogenic Candidate Genes Predict the Development of Secondary Lymphedema following Breast Cancer Surgery. PLoS One. 2013. 8(4):e60164.
- Photo courtesy of SteadyHealth