Chronic subdural hematomas are relatively common neurological conditions that can be seen secondary to chronic alcohol use, chronic pain-killer use or when dealing with cases of head trauma. In a good portion of these cases, some complications can lead to re-bleeding events or cerebrospinal fluid entrapment that can lead to altered mental status if the condition is not alleviated. Chronic subdural hematomas is a condition that is more prevalent as a patient ages and studies show that about 3 percent of patients over the age of 80 will suffer from them. [1]
Although the cascade of symptoms can be quite complex for this condition, the treatment option has always been quite straightforward. Burr hole surgery is the standard of care and essentially means that a small hole will be drilled into the surface of the skull in order to drain the blood that had been collected in the subdural space and evacuated to prevent from increased intracranial pressure. The question is if this is the best possible method available or is there an alternative treatment that can be just as effective.
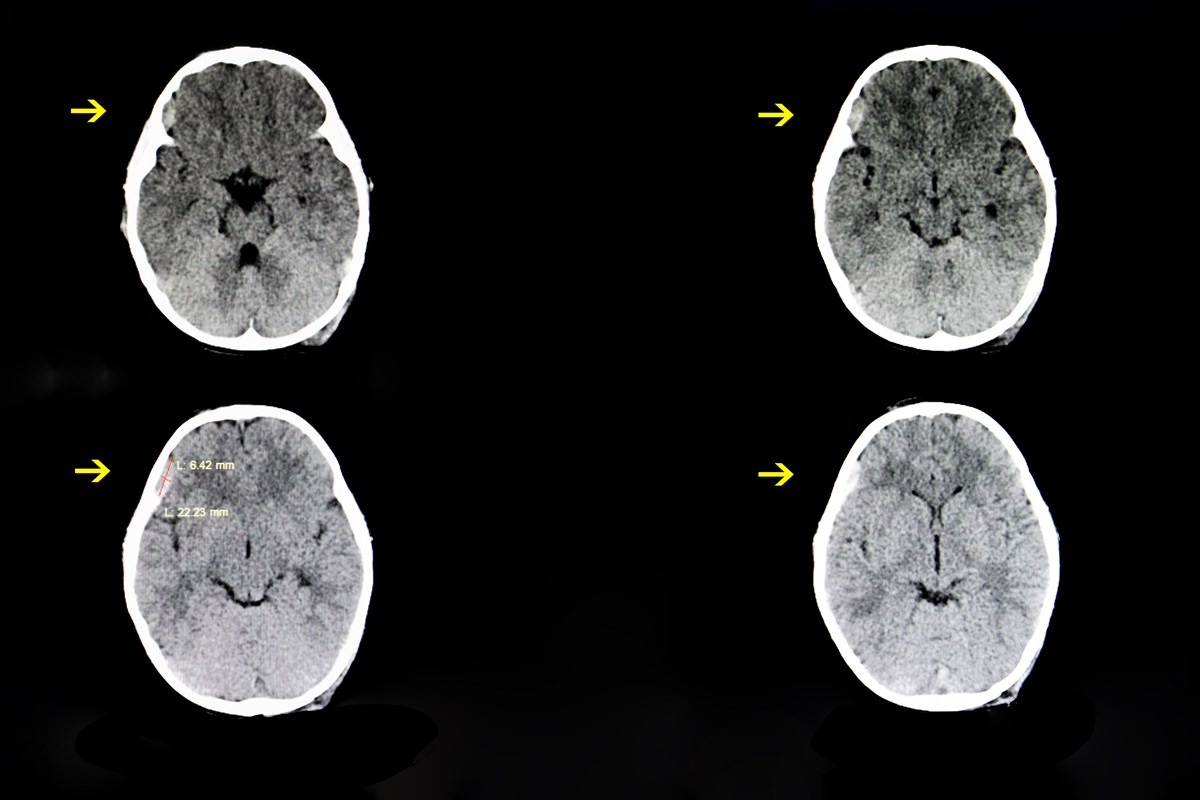
Burr hole procedures are valuable in the clinical setting because they provide a quick solution to the underlying pathology and have been shown in studies to have low recurrent rates so patients will not need to have another operation in the future most of the time. Although there is some debate in medical circles about what type of drill bit and what location provides the best outcome for the patients, they determined that having a catheter placed on the frontal bones of the skull offered the best response rate. [2]
The radical nature of this procedure has left many patients and families hoping for a more conservative approach to manage subdural hematomas, and the medical community has not been deaf to these requests. When surgery is necessary, patients are now able to have newer craniotomy procedures called trephination where smaller holes and catheters are needed. This procedure results in a reducing in the possible bleeding secondary to the surgery the patient just had so it is much more attractive for patients and currently, about 85 percent of patients will have this type of operation when dealing with subdural hematomas.
Current data shows that this minimal technique is not as effective as a more cumbersome craniotomy and patients will have longer hospital stays, are more prone to infections and are likely to need another operation. For this reason, traditional craniotomies are the better option for patients concerning surgical decisions.
The risk of conservative therapy instead of surgery is that patients will need to take anticoagulation therapy to prevent brain clots and strokes from occurring. Studies indicate that the risk of subdural hematomas increases nearly 50 times more in patients taking anticoagulation medication compared to patients not on anticoagulation so you are making the problem much more dangerous for the patients if surgery is not done as soon as possible.
Patients taking this type of anticoagulation therapy may actually worsen their prognosis because doctors will need to waste time waiting for blood levels to drop before they can begin the surgery and this could take multiple days depending on the dose of the medication. It is much better for the patient's prognosis to just go for a craniotomy to try to stop the bleeding as soon as possible. [3]
- 1.) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3821407/
- 2.) https://www.ncbi.nlm.nih.gov/pubmed/24995782
- 3.) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4556906/
- Photo courtesy of SteadyHealth