Anyone else had this? Any tips on how i can ease the soreness? Its when im at work it bothers me the most. Thanks x
Loading...
Nicz30 - You don't say what operation you have had? An obvious suggestion would be try and pat dry and not rub, also to shower yourself clean when you can. Sometimes soreness is because of thrush near a wound site. Without knowing more about your circumstance difficult to say. PRobably best to see a nurse (they are often better at advising at these sort of issues - healing, soreness - than doctors). Don't leave it though as it might develop into an infection. SOrry I can't help more.
Hope everyone else is OK.
Loading...
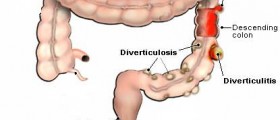
My colon resection was successful, one thing I found out which I thought was interesting.....stitching together bowels have a higher chance of fistulas developing that stapling.....so...has all these stitching together my fistula been in vain? who knows. But I will say one thing.....A colostomy is not the end of the world, I had a temp one and without it, my big fistula would have NEVER healed, I wish now I had one when this all started 2 years ago. Now I am patiency waiting for the small rvf to heal now that the Crohns is bac under control.
Flower
Loading...
To the previous military spouse that posted earlier, I absolutely agree that you must fight for a civilian referral but I'll go one step further. My first civilian referral was an over-confident jerk that swore he'd had experience fixing rvfs--not true. So I finally demanded a well-established CRS with published work and copious experience with rvfs. It was a big fight with Tricare but I got my referral. Now despite the fact that this recent surgery with this expert has not yet panned out, I still felt better cared for and he has other options that I may consider. Proper tests were done (big clue to ditch a crs if they don't recommend any ultrasounds or the like before scheduling a surgery) and this CRS listened to my symptoms without explaining away what I KNEW what happening. Don't go to the local CRS!!!
All in all, if my new rvf is small enough, I might consider doing a reversal and live that way which is exactly how I started off before 6 surgeries and a lifetime's worth of disppointment...I would suggest if someone only has minor gas issues to not go through surgery. The ileostomy has been a big emotional issue for me because I think it interferes too much with me being a young mother. I haven't properly squeezed and hugged my kids since I got the bag. But that's me. If I had a bag to save my life from cancer or something like that, I'd feel differently.
I'll let you know if my new tract closes or what the choice for me will be but I love all of you for being here and being so brave to live with this condition and yet smile at your neighbor! We're good people with a heavy emotional burden but I'll keep trying if you will.
-Posie
Loading...
Sorry to hear your news but all may not be lost. You never there may still be some healing especially as you have the ileostomy. Why is it we have to constantly go through all this? I'm glad to hear from you but not with this news.
I seemed to have swapped an RVF for an anal fistula and I am constantly battling an infection. I feel tired all the time. I never had that with an RVF. Like you - if I could get a small RVF only I'd take that and live with the consequences. I almost wish I'd never had the surgery but once you start it is difficult to stop.
Bea
xx
Loading...
HI Everyone,
I've read a few of the posts and wanted to share my story and get some advice.
I gave birth to a 7lb 6oz girl in Feb 2010. My doc had to use the vacuum to get her out fast because she had the cord around her neck. She wasn't very big so I am still not sure why I ended up with a episiotomy and 4 degree tear.
Anyway, two days after coming home from the hospital I noticed gas passing through the wrong hole. I'm a in internet junkie so I immediately researched this and knew then that I had an RVF, although I've never had stool come through. I went to my Ob that delivered my daughter two weeks after giving birth and she said the air passing could be just because I am still healing and it should go away.
At my 6 week check the problem was still there so my doc scheduled a perineum repair surgery, basically she just gave me another episiotomy and re-stitched me up. While the stitches were in I did not have the gas passing through the wrong hole, but I could feel the pressure of it trying to break through. Once the stitches dissolved the problem came back so my OB sent me to a vaginal reconstruction surgeon. She did the blue dye test and found the RVF, she said it was the size of the tip of a dull pencil. She was going to do a full vaginal reconstruction but sent me to a colorectal surgeon to check it out from the "other side." The colorectal surgeon said I didn't need a vaginal reconstruciton, but that he could do an advancement flap that should solve the problem.
I am now one week and one day post-op from an advancement flap repair. Two days after the surgery, I started feeling the gas come out of the wrong hole again. Yesterday, I saw the colorectal surgeon and told him about it, he said it's because I am still healing and said the vaginal wall feels strong and that he would recheck me in 2 weeks. He didn't check rectally because he didn't want to disturb things.
I really hope it heals because I am starting to feel really sad that this surgery didn't seem to work. I can hold my gas in by contracting my sphincter muscles and I wasn't able to do that before the surgery. Does anyone have any words of advice/encouragement? Is it too early to be worried about the gas coming through the wrong hole already?
Is there anything I can do to help it heal/close-up? The doctor's orders were to not eat solids for 4 days after the surgery (I did that), to not exercise for 3 weeks, to not have sex for 4 weeks, and to take a stool softener. Is there anything else I can do? I read in some posts that people were instructed not to lift heavy things after their surgeries. I was not instructed to do this and have been lifting by daughter (21 lbs), wondering if I should stop or if the damage is done.
I really don't want to have another surgery. Your advice is appreciated. Thanks.
-SRB
p.s. I plan to have at least one more child, and all of the doctor's I've seen have told me to either finish my family before having the RVF repaired, or to have it repaired and have C-sections.
Loading...
Sorry to hear your story. I think the last thnig you wrote is certainly true - don't have another vaginal birth if you get the RVF fixed beforehand as it will risk a recurrence and they are difficult to fix.
The general tips/advice which I think others would back up are:
(1) Despite how it was caused this is now a bowel problem - a gynaecologist is no good at fixing it
(2) Get the best doctor you can as soon as you can
(3) Re (2) The more surgery you have the more scar tissue you get - each attempt (if it fails) makes the chances of the next operation working less - hence throw the best at it from the start.
(4) One issue in healing not working is the bowel continuing to operate - both the muscles moving and the contents of the bowel make healing difficult.
(5) Re (4) - a temporary colostomy or ileostomy removes a lot of these issues and promotes healing in the affected area - given the number of attempts to repair is not endless do not put off having a temporary colostomy - consider it certainly after two repair attempts have failed.
(6) TEchniques will be advancement flap (which you have had) mainly but depending: an anal spinchter muscle repair or a Martius type
graft. I am sure there are others but these seem to be main ones.
Also think hard about what you can live with. I have had 5 operations. At the beginning my sphincter muscles were in tact and working fine. They are now compromised by surgery. I don't know when I have a reversal what cotnrol I may have - if I opt for further repairs I may become completely in continent and require a permanent colostomy. For me remaining continent is now as much of an issue as getting repaired. I might be a bad case scenario, but if your current repair doesn't fix then you might end up with several attempts.
From what you say there is still chance of healing (if no stool comes through). I think not lifting is good advice - though I also was not advised of this. THose of us who have been through many operation would be delighted to have good sphincter muscles and 'only' have gas coming through. It's not much comfort and I,m not saying I wouldn't do the surgery again - but do think about it and if you can bear it - read more of the posts on this site.
GOod luck - keep posting esp if you fel bad. One of the worse things about the RVF is how it gets you down and make you feel un-female etc.
Bea
Loading...
Hi Again,
Bea, thank you for the advice and words of encouragement. I did read some more of the posts and I have a lot of sympathy for what we are all going through. The posts made me feel better knowing that I am not alone with this issue, but they also made me sad seeing that there are so many and there have been very few complete recoveries.
As an update, I had a small bowl movement this morning and when I wiped there was stool on the toilet paper. I am very sad about this new development, but trying to stay hopeful that maybe it will stop as I continue to heal. But my honest feeling is telling me that not only did the surgery fail, the fisutla is now bigger because I never had stool coming through before. I called the doctor to tell him about it and his nurse said that I should come in ASAP. So I'm going in today. Trying not to get too upset (it's difficult) as this is not the end of the world, but hoping that something can be done.
I can't afford to have another surgery. And I can't take so much time off from work and school and running my house. Feeling real disappointed today.
-SRB
Loading...
**Update** Went to the doc, he said that a piece of the graft pulled away from the fistula, some of the graft is still there but a small piece of the fistula, about this big >> O<< is what remains uncovered. Seems silly to me that a fistula that small can let stool through. Doc gave me a scrip for antibiotics and said to bulk up my stool. I guess I was only supposed to be on the softner for 3 days after the surgery, but I kept taking it. Going back in in two weeks, he said I have 50/50 chance of the small hole closing up on its own. But if not he wants to do another flap surgery. I hope it heals. Wish me luck!
-SRB
Loading...
Sorry to hear your news. I think that now the stool is coming through it is unlikely that it will heal on it's own. Bacteria in the stool cause infection and infection stops healing. Plus it is in effect dirt in the wound. I won't say it's impossible but unlikely. The anitbiotics will give it the best chance. I am so sorry for you as the stool coming through is the most soul destroying thing and the anguish of failed surgery is something which is unbearable at times. I and others had the first surgery making things worse. I would seriously suggest that you re-consider continuing with the current doctor. Ask them how many of these operations they have done and their success rate. You say you can't afford another operation at the moment - I don't think waiting will make it any worse and might give you time to research and get a better doctor. As I said before, a colostomy might be necessary. I hate having to say these things to you, as some people do fix quite easily and I might seem negative but I'm trying to help you get the best treatment for you. It would be worth waiting to be seen by someone really good.
I really feel for you. Reading your post took me back to my failed ops ... the dread of going to the toilet and what you might see. I feel sick at the memory of it. If you can try and find a way of being hopeful but realistic that is best but difficult to achieve. Let us know how you progress.
Good luck.
BTW - I currently have an anal fistula (this replaced the RVF at the last operation) with a seton stitch in it to aid 'healing' which means - allow the pus to drain (you wouldn't believe how much pus I get coming out of such a small hole - anal fistulas are very different I am finding). I have an ongoing infection which leaves me very tired all the time. I have to wait for this to clear up, it's already taken 5 months but apparently it should clear up eventually ..... it's a waiting game at the moment. Then I might have a reversal and see how my body functions.
Bea
Loading...
Loading...
Loading...
srb - it is sad the others don't post now but I guess they have mosly stopped having surgery and are getting on livign as best they can with their bodies as they are. most either have control issues or small fistula still but we are the hard cases. There have been good news stories too.
Colostomy is OK - you get used to it and learn to manage things. I work, salsa dance etc. You can swim (I haven't because I have an infection in the fistula but it is not the colstomy which stops me).I haven't got a partner since the colostomy but people say it is fine - you can get caps or small pouches which make it less intrusive for intimate moments.
I do find clothes a problem - my stomach seems slightly bigger with it and for work in particualr I wear long looose tops so that if the bag fills in a meeting etc it isn't obvious.
It sounds like your CRS is OK but even so they may not specialise in this type of operation. so do ask how many times they have done it and success rates etc.
2guest - SOrry to hear your news. Do feel free to vent on this site. It's difficult to talk the about symptoms to others. Where about are you? UK? USA? I'm in the UK so can't help much if in USA ....
Bea
Loading...
Loading...
Very sorry to hear your story - especially about the surgery from someone apparently not really knowing what they are doing. Even if they have admitted it now.
I think that you will need an endo anal ultrasound to confirm where the holes are on your bowels/rectum/anus and also to check your anal spinchter muscles. This involves a probe going up your beck passage - not very deeply. It shouldn't hurt - the probe is like the size of a thick finger. Also expect some physiology tests. These i've only had once but is a few ( between 2 and 5) different test to look at your muscle control. These are slightly odd but not at all painful and really just leaves you wondering what they are learning. I would also hope any doctor worth his or her salt would examine you digitally (finger up back passage) and also with a telescope. THe finger can not be beaten for feeling small holes and quality of tissue. The telescope with a light helps them to see if it is inflamed. My current surgeon also examines my vagina digitally but lying on my side in the same position as a rectal exam. I have heard of a dye test where dye is put in the back passage and a tampon in the vagina will pick up the dye if there is a connection. This can help prove a hole in the vagina. You will not believe how many doctors think you are just mistaken - you've lived all your life and never thought you had stool coming out of your vagina - you aren't suddenly going to make it up - but they sometimes seem to think you aren't wiping properly etc. ANother test is a very liquid type of barium meal in the back passage and then an x ray. This can help show the internal passage of the fistula. I think this last one prob not neceesary for you at this stage.
Another one is having an MRI scan - I've has 3 and they never show anything for me - but again it might be used.
That's the most likely tests. None are really invasive or painful - just mildly embarrassing sometimes and perhaps a touch uncomfortable. The doctor might want to do a colonoscopy to check the bowel higher up as well - this is often doen under sedation. AGain, this is not essential, but if they want to do it all well and good.
I also had a terrible first repair experience - not as bad as yours but along the same lines. I think that you almost certainly need a colostomy temporarily to give your body a chance to heal. I've got one and it could be worse. It's not the end of the world.
I'd suggest to try and read as many posts on this blog as you can to get an idea of the range of experience.
THat's all for now - I'll try and post when I can - not always very regular.
Good luck and I hope things improve from here on in. Questions for the doctor:
How many repairs have you done? What is your success rate? What are my chances of success? If he doesn't mention a colostomy ask about it.
ASk about the risks - the damage to your spinchter muscles in aprticular and the risk that you may not have control going forward. THis is my issue now - and I am going to have to live with a hole going forward but can't risk more surgery otherwise I might be incontinent.
BEa
Loading...