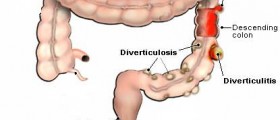
A lower anterior resection is the surgical removal of the upper two-thirds of the rectum, leaving the anal sphincter intact. You may see the procedure referred to by older terminology, anterior resection of the rectum or simply as anterior resection. This procedure is used to treat rectal cancer and in some cases of diverticulosis. The procedure is sometimes used to treat severe roundworm infestations, extremely numerous polyps, gangrene of the bowel, complications of radiation therapy for colon cancer, Crohn's disease, ulcerative colitis, inflammatory bowel disease, Hirschprung disease, extreme constipation (obstipation), or traumatic injuries to the rectum.
It is an alternative to a more drastic procedure called abdominoperineal resection, which removes the anal sphincter and rectum and part of the sigmoid colon, with permanent placement of a colostomy bag. Lower anterior resection is reversed by a procedure called anastomosis, reattaching the distal (lower) rectum to the rest of the bowel so the temporary colostomy bag can be removed.

That's where the procedure often goes wrong. Common complications of the procedure to reverse the resection include:
- Leaks,
- Bleeding,
- Infection,
- Stricture, and
- Ileus, an inability to push stool outward, especially when the procedure is performed on children.
- If you are well enough to discuss the procedure with your doctor before it is performed, inquire whether the doctor will hand-sew the stitches or use staples. Hand-sewn stitches are sometimes used when the doctor is more concerned about ileus. Staples are sometimes used when the doctor is more concerned about leakage. Your doctor's concerns may be a clue as to when everyone needs to be on the lookout for complications.
- Make sure you are not dismissed from the hospital too soon. Close medical attention, at least during the inflammation phase, is a must.
- Expect changes in your bowel movements after the surgery. You may find that bowel movements tend to "cluster." You may feel that you "still need to go" after a bowel movement, but you probably will.
- Certain foods may cause you to need to go to the toilet immediately after eating after you have had your surgery. They may also cause abdominal pain until you are able to defecate. Pay attention to what you eat and avoid these foods.
- Be sure to drink 6 to 8 glasses (1.5 to 2.0 liters) of water every day. Caffeinated beverages are OK unless your doctor says otherwise, but they do not count as "water" for this purpose.
- Eat high-fiber foods every day. They feed the probiotic bacteria that give bulk to the stool and make bowel movement easier.
- Barone JE. Abnormal vital signs not a good indicator of anastomotic leaks. Medscape Medical News. March Guenaga KK, Matos D, Wille-Jørgensen P. Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev. 2009. (1):CD001544.,24, 2014.
- Photo courtesy of SteadyHealth