A recent Japanese study has found that statins stimulate artherosclerosis and can cause heart failure. As a result the researchers from Nagoya City University and the Institute for Consumer Science and Human Life at Kinjo Gakuin University have proposed that the current guidelines for statin treatment be “critically re-evaluated.”
Since statins were first introduced in the 1990s, the most commonly propounded theory is that they decrease cholesterol and therefore also decrease atherosclerosis. But the Japanese researchers set out to prove that statins can cause calcification in the coronary arteries and can also inhibit the synthesis of vitamin K2 which is “the cofactor for matrix Gla-protein activation,” a vital key in the chain to protecting the arteries from the calcification that kills so many people.
This occurs as a result of the depletion of coenzyme Q10 (see below) and heme A (a biomolecule that is produced naturally, and which is essential for respiration), and thereby the generation of adenosine triphosphate (ATP).

The Importance of Coenzyme Q10
Coenzyme Q10 is known to be a vital factor when it comes to mitochondrial respiration. It also has important antioxidant properties. When there are deficiencies of this coenzyme, various myopathic and neurologic syndromes may occur. A study undertaken by medical doctors at the Ochsner Clinic Foundation in New Orleans, Louisiana in 2010 identified “statin-induced mitochondrial dysfunction” caused by a lack of coenzyme Q10. Specifically, they found that statins “interfere with” production of mevalonic acid, a precursor in the synthesis of coenzyme Q10. In their report published in The Oschsner Journal, they state that statin medications “routinely” result in lower coenzyme Q10 in “the serum,” and sometimes in muscle tissue as well.
In the Japanese study paper published online in the National Institutes of Health (NIH) US National Library of Medicine in March 2015, H. Okuyama et al state that statins impede muscle function in blood and heart vessels because coenzyme Q10, heme A and ATP generation are depleted. Additionally, they say statins tend to prevent proteins that contain selenium from being biosynthesized.
The Importance of Selenium
Selenium occurs in proteins in the form of selenocysteine, an amino acid that is essential for human health. A number of biochemical and nutritional studies have implicated it in numerous biological processes including immunological function. Some selenoproteins have been found to play a “chemopreventive role” in cancer of the prostate, colon and lungs. So if it cannot be biosynthesized for some reason, this could impact negatively on our health.
The Japanese study concluded that impaired selenoprotein biosynthesis might be a factor leading to congestive heart failure, stating that the effects were similar to the “dilated cardiomyopathies” identified in cases of selenium deficiency.
“Thus, the epidemic of heart failure and atherosclerosis that plagues the modern world may paradoxically be aggravated by the pervasive use of statin drugs.”
The Ugly Side of Statins
While there seems to be more positive information about statins than negative data, when cardio-vascular specialists berate the benefits of statins, it is surely time to take note, if not action.
For instance, in 2013, two doctors, Sherif Sultan and Niamh Hynes published a paper in the Open Journal of Endocrine and Metabolic Diseases titled The Ugly Side of Statins. Systemic Appraisal of the Contemporary Un-Known Unknowns. Sultan is a senior medic and Hynes a surgeon from the University College Hospital Galway and Galway Clinic’s Departments of Vascular and Endovascular Surgery in Galway, Ireland. They cite 39 published research reports dating from 2002 to 2012, one of which is their own. Their findings are alarming.
Warning that “naïve indiscriminate acceptance of novel mainstream therapies” was not always advisable they state that statins might be “causing more damage than good.”
READ Statins: Advantages And Limitations
Sultan and Hynes examined research reports and the results of more than 55 trials on statin therapy and found there had been no significant reduction in the risk factors (mainly cholesterol and blood pressure) relating to coronary heart disease (CHD). While they found that in some cases statins might improve a sick patient’s quality of life, they identified a number of major adverse effects that they said had been “under-reported.” Worse still, the way in which these negative effects had been withheld and even concealed from the public was, they said, “a scientific farce.”
Sultan and Hynes found that all side effects of statins were dose dependent and persisted throughout treatment. Those being treated with statins faced some alarming risks, they said. These include:
- Diabetes mellitus, erectile dysfunction, and the formation of cataract in young patients.
- Cancer and neurodegenerative disorders as well as a myriad of infectious diseases in elderly patients.
- Cardiovascular problems in women, young patients, and those suffering from diabetes mellitus.
Additionally, statins were associated with three times the risk of aortic and coronary artery calcification.
Lifestyle Changes Are More Effective Than Statins
While various institutions including the American Heart Association, American College of Cardiology, and medics at Harvard Medical School persist in recommending statins for those at risk of having stroke or a heart attack, there is no doubt that lifestyle changes are more effective than statins. The only issue is that not everyone believes in exactly the same lifestyle changes, particularly when it comes to diet.
That said, as long ago as 1956, the three major risk factors for cardiovascular disease (CVD) had been identified as high blood pressure; increased serum cholesterol levels; and smoking.
Recommended Lifestyle Changes
After their comprehensive review of various trials, Sultan and Hynes were convinced that the best way to prevent primary cardiovascular problems and approach regeneration programs was to make lifestyle changes, including abstinence from smoking tobacco. This, they concluded, had “enhanced clinical efficacy” and improved quality of life more than any pharmaceutical or other so-called “conventional” intervention was capable of.
While the British Heart Foundation continues to promote statins, it does (somewhat casually) warn against potential side effects. It also advises that there are other ways to lower cholesterol – which is, of course, why doctors prescribe statins (see below). You can do this, they say, by:
- Eating a balanced and healthy diet
- Maintaining a healthy weight, taking your body mass index (BMI) and waist circumference into account
- Making sure you do physical exercise regularly
The Mayo Clinic, which appears to be as pro statins as the institutions mentioned above, state that “doctors are far from knowing everything about statins.” However they also state unequivocally that, “lifestyle is still key for preventing heart disease,” and promote the fact that lifestyle changes are vital to reduce the risks of heart disease. Their recommendations are very similar to those of the British Heart Foundation:
- Eat a healthy diet
- Maintain a healthy size – specifically in terms of “waist girth.” This, they say should be less than 35 inches (about 89 cm) in women and 40 inches (not much more than a meter) in men
- Exercise regularly, sit less, and generally ensure you are physically active
- Stop smoking and be sure to avoid “secondhand smoke.”
Reliable dietary recommendations remain contradictory, especially in terms of high fat versus low fat, and the value versus potentially harmful effects of grains. Generally, though, it is now agreed that carbohydrates should be limited, and sugar largely avoided.
Cholesterol and Statins: How It All Started
American physiologist, Dr Ancel Keys established a link between dietary cholesterol and atherosclerosis and cardiovascular disease more the 60 years ago. He blamed dietary saturated fat, and blazed a trail for low-fat diets and the development of drug therapy that eventually led to the launch of statins in the 1990s. He believed that lipids (essentially various forms of fat) needed to be decreased in the human body, but also advocated a healthy lifestyle (albeit one that included minimal fat) along with regular exercise.
Nicknamed “Mr Cholestrol,” Keys began studying a link between diet and cardiovascular disease after World War II when he realized that food shortages in Europe seemed to correlate with a drop in coronary artery disease (CAD.) This culminated in his famous (infamous to some) Seven Countries Study that found, amongst other things that a typical Mediterranean diet resulted in low blood cholesterol and hardly any heart attacks. It also found that where fat was generally a major component in meals (especially in the US and Finland,) heart-attack death rates and blood cholesterol levels were highest.
The first trials looked at drug therapy and/or diet and its effect in preventing CVD. Dietary modification was largely focused on reducing total (and more specifically saturated) fat content, with some trials looking at using soybean and corn instead of the usual oils (sunflower, canola and so on.)
From mid 1990, mega-trials started focusing on statins that could lower lipid levels. Sultan and Hynes refer to this as the “statin saga,” which is what they label a “marketing trap” that has really only benefited middle-aged men who were already suffering from CHD. Ironically, though, statins aren’t even proven to be the best form of primary prevention for them either. Aspirin, they say, has proved to be a better form of primary prevention. Also, they reveal that high cholesterol has been found to protect the health of heart failure patients and the elderly.
As they point out, the statin industry and spin-offs are (or were when the study was published in 2013) worth 20-billion a year (the currency is not specified, but presumably they mean £20 billion.) Furthermore, this is part of what they describe as the “utmost medical tragedy of all times.”
As Sultan and Hynes’ paper states, it isn’t just that the healthcare industry has managed to “inadvertently” induce potentially fatal nutrient deficiencies in millions of people who were otherwise healthy. It is also the fact that the industry has not reported on all the negative side effects that result from taking statins, and there has been active discouragement in terms of publication of the many negative studies that have been done.
- www.bcmj.org/article/ancel-keys-and-lipid-hypothesis-early-breakthroughs-current-management-dyslipidemia
- www.ncbi.nlm.nih.gov/pubmed/25655639
- www.ncbi.nlm.nih.gov/pmc/articles/PMC3096178/
- www.jbc.org/content/273/15/8910.full
- file.scirp.org/Html/3-1980073_34065.htm
- www.health.harvard.edu/blog/cholesterol-and-statins-its-no-longer-just-about-the-numbers-201311136868
- www.bhf.org.uk/heart-health/treatments/statins
- file.scirp.org/Html/3-1980073_34065.htm
- Photograph of statins courtesy of AJ Cann/Flickr
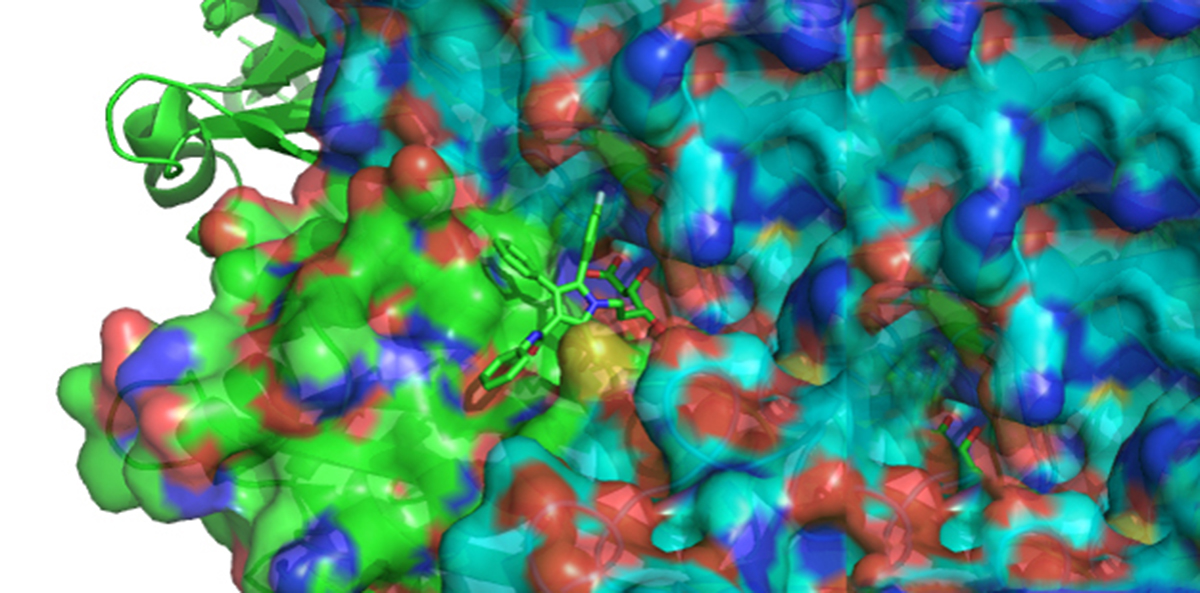
- Photograph of atorvastatin binding courtesy of A2-33/Wikimedia Commons
- Photo courtesy of
- Photo courtesy of
- Important notification about information and brand names http://www.steadyhealth.com/polices/terms-of-use#copyright

