Spending a substantial amount of time in ICU can result in physical issues such as urinary tract infections, stasis pneumonia, adult respiratory distress syndrome (ARDS), deep venous thrombosis (DVT) with possible embolism of the pulmonary arteries and bed-sores.
The study
Researchers conducted a multi-institutional study on a national level, which consisted of over 700 participants who had survived life-threatening situations and who had spent time in an ICU.
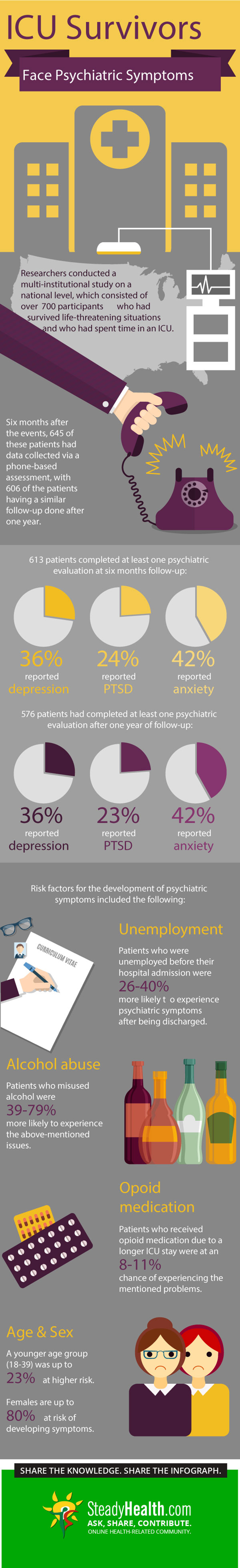
Six months after the events, 645 of these patients had data collected via a phone-based assessment, with 606 of the patients having a similar follow-up done after one year. 613 patients completed at least one psychiatric evaluation at six months follow-up, and 576 patients had completed at least one psychiatric evaluation after one year of follow-up.
An important limitation which needs to be addressed, is that only patients who had suffered from ARDS were included in this study. The risks mentioned therefore may not be applicable to patients who had other problems in the ICU.
The findings
The findings showed that, based on the self-reporting done at six months, 36% of the participating patients had shows signs of major depression. At the same follow-up time, 24% of patients had reported signs of PTSD and 42% exhibited signs of anxiety. At one year follow-up, the prevalence of these symptoms was nearly the same at 36%, 23% and 42%, respectively.
READ Anxiety, Nervousness? How To Work It Out Mentally And Physically
Various other aspects were looked at in determining which of these would be classified as risk factors for the development of psychiatric symptoms after surviving a life-threatening illness and spending time in an ICU. These included the following:
- Patients who were unemployed before their hospital admission were 26-40% more likely to experience psychiatric symptoms after being discharged.
- Patients who misused alcohol were 39-79% more likely to experience the above-mentioned issues.
- Patients who received opioid medication due to a longer ICU stay were at an 8-11% chance of experiencing the mentioned problems.
- A younger age group (18-39) was up to 23% at risk of these issues.
- Females are up to 80% at risk of developing symptoms.
The clinical significance
Adult Respiratory Distress Syndrome
ARDS develops when the small, elastic air sacs in the lungs, called alveoli, fill up with fluid. This occurs when the protective membrane of these alveoli become compromised due to inflammatory changes which occur under certain situations.
When the alveoli are filled with fluid, then oxygen can't be transported from the lungs to the bloodstream of the body. This problem is most probably the most common complication in critically ill patients or those who have sustained injuries which compromise their breathing.
The prognosis of patients with ARDS varies depending on the patient's age and how ill they are. It can therefore vary from the patient recovering completely to being fatal.
High risk patients for ARDS would then include those who are hospitalized, are critically ill and have sepsis, as well as those who have a chronic history of alcohol misuse.
Causes
These are the most common associated causes or ARDS:
- Severe pneumonia - this condition can affect all collective five lobes of the lungs.
- Breathing in of certain substances - inhaling high concentrations of chemical fumes or smoke can lead to ARDS.
- Aspiration - inhaling vomit or other stomach contents can cause issues such as aspiration pneumonia which complicates to ARDS.
- Major injuries - injuries, especially those involving the chest and the head, can result in ARDS due to direct damage to the lungs and the area of the brain involved with breathing, respectively.
Symptoms
The intensity of the symptoms of ARDS can vary depending on what the cause is, as well as how severely the lungs are affected. These can include the following:
- Severe shortness of breath (dyspnoea).
- Extreme tiredness and confusion.
- Unusually rapid and laboured breathing.
- Low blood pressure (hypotension).
READ Anxiety, Depression and Self-Abandonment
Complications
As mentioned, some patients can recover completely from ARDS. There are patients however who do develop complications, and these can include the following issues:
- Pneumothorax - ventilators are used to help the patient breath and at the same time apply pressure on the fluid in the alveoli so that it can be driven out of the lungs. These machines can unfortunately exert pressure, which forces gas through the outer membrane of the lung, and cause it to collapse.
- Pulmonary fibrosis - thickening or scarring of the tissue between the air sacs can occur a few weeks after ARDS developed in the patient. This can result in the lungs becoming stiffer which makes oxygen transport to the bloodstream more difficult.
- Infections - pneumonia can occur due to bacteria breeding in the airway secretions which can be transferred from the intubated pipe in the trachea to the lung tissue.
- Thromboembolic events - lying still in a bed while attached to a ventilator can increase the chances of developing clots in the deep venous system of the lower legs. These clots can then break off and lodge in the pulmonary arteries thus obstructing blood flow to the lungs.
- Cognitive, memory and emotional issues - ARDS can lead to low oxygen levels in the body and therefore compromise oxygen to the brain. This can result in cognitive issues and memory loss in these patients. These patients also report going through a period of depression.
- www.medicalbrief.co.za/archives/icu-survivors-face-high-risk-of-psychiatric-symptoms/
- www.mayoclinic.org/diseases-conditions/ards/basics/definition/con-20030070
- Photo courtesy of
- Photo courtesy of
- Photo courtesy of
- Photo courtesy of
- Photo courtesy of
- Photo courtesy of


Your thoughts on this