Because women with PCOS have higher androgen and estrogen levels but are lower on progesterone, and because they're likely to ovulate less often, polycystic ovary syndrome is one of the risk factors for endometrial cancer. A study of over 10,000 Danish PCOS patients indicated that PCOS may quadruple your odds of developing this kind of cancer, which begins in the cells that line the uterus.
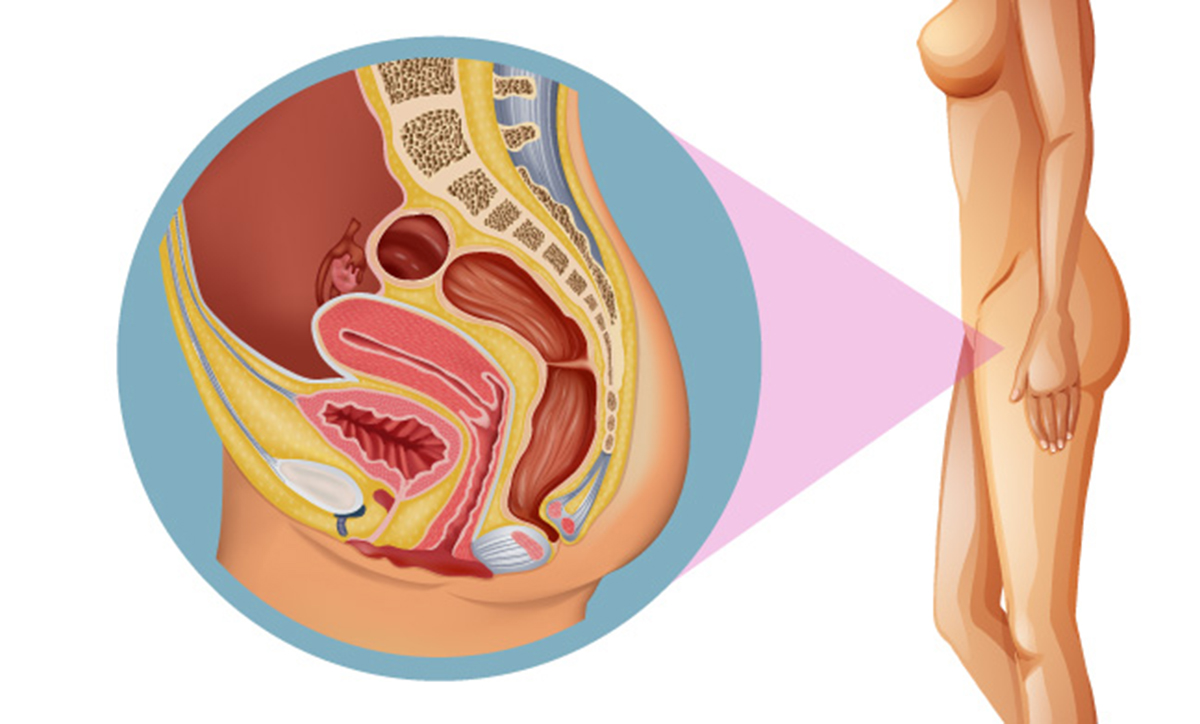
1. What is endometrial cancer?
Endometrial cancer is one of several kinds of cancer that start within the uterus (or womb). It begins within the cells of the endometrium, the lining of the uterus. Endometrial cancer is the most frequent cancer of the female reproductive organs in the United States, with over 60 thousand new diagnoses made each year. This kind of cancer affects postmenopausal women more often, though younger women can also develop it.
2. Endometrial cancer: Remember the symptoms
Always see your doctor if you notice the following symptoms, which can point to endometrial cancer:
- Vaginal bleeding or spotting between periods
- Vaginal bleeding or spotting after you have entered the menopause
- Changes in vaginal discharge — particularly watery or bloody discharge
- Pelvic pain
- Spontaneous weight loss
- Feeling a mass in your pelvis
3. Endometrial cancer: Risk factors
PCOS is a risk factor for endometrial cancer because it causes high estrogen and androgen levels relative to your levels of the hormone progesterone. Other known risk factors for endometrial cancer include:
- Having more periods in your lifetime — because you experienced menarche early or entered the menopause late, for instance
- Not having experienced any pregnancies
- Hormone therapy for breast cancer — tamoxifen
- Being obese
- Age — your risk goes up with time
- A personal or family history of endometrial, ovarian, breast, or colorectal cancer
4. How strong is the link between PCOS and endometrial cancer?
A large Danish study found that women with PCOS have four times the risk of developing endometrial cancer, but further research still needs to be conducted before it is clear how strong the link between the two conditions is. If you have PCOS and are worried about endometrial cancer, the best thing you can do are to:
- Make proactive changes to reduce your risk — more about that in a while
- See your doctor regularly
- Seek medical attention right away if you notice any of the possible symptoms of endometrial cancer, particularly abnormal vaginal bleeding
5. How is endometrial cancer diagnosed?
After you see your doctor because of symptoms you're worried about, they will do a pelvic examination and may order the following tests:
- A transvaginal ultrasound
- A hysteroscopy, which also allows your doctor a closer look at your uterus
- Blood and urine tests
- PAP smears can also find certain kinds of endometrial cancer
6. The treatment of endometrial cancer
Women diagnosed with endometrial cancer may be treated in a variety of ways, and they include:
- A hysterectomy, often in combination with a salpingo-oophorectomy — the uterus, cervix, ovaries, and fallopian tubes are removed.
- Chemotherapy.
- Radiation therapy.
- Hormone therapy.
7. Reducing your risk of endometrial cancer
If you have PCOS, and especially if you also have other risk factors for endometrial cancer like being obese or having diabetes, you can take a number of steps that will help you lower your risk and help you improve your prognosis should you develop it. That includes seeing your gynecologist regularly, including for PAP smears, and making sure that you receive treatment for your PCOS.
It is also important to either maintain a healthy weight or try to get there if you are currently overweight or obese, as most PCOS patients in the US are. This is because obesity leads to higher estrogen levels, something that makes you much more vulnerable to endometrial cancer.
Diet and exercise both play important roles in weight reduction and maintenance, of course — but they also contribute to a lower risk of endometrial cancer independently. Because diets rich in saturated and trans fats raise your cancer risk by affecting the way your body processes estrogen, a low-fat diet is beneficial. Regular exercise, meanwhile, has also been found to reduce the risk of endometrial and other cancers.
In your reproductive years, you may want to consider using hormonal contraceptives when you are not trying to get pregnant. Birth control pills lead to more regular periods and reduce symptoms of PCOS like hirsutism and acne, but they also lower your risk of endometrial cancer. This protective effect stays with you for a few years after you stop using birth control pills. The copper IUD (Paragard in the US), which doesn't emit hormones, seems to lower the risk of endometrial cancer for reasons that aren't quite clear yet, too.
During the perimenopause and once you've entered the menopause, make sure to discuss the pros and cons of using hormone replacement therapy with your doctor in detail before even considering it. Research has shown that HRT increases your risk of several cancers, including endometrial cancer.
- Gottschau, M., Kjaer, S. K., Jensen, A., Munk, C., & Mellemkjaer, L. (2015). Risk of cancer among women with polycystic ovary syndrome: A Danish cohort study. Gynecologic Oncology, 136(1), 99–103.
- Photo courtesy of
- Photo courtesy of


Your thoughts on this