Testosterone is the most important androgen (male sex hormone); by definition, androgens are responsible for the development of male sexual characteristics.

Testosterone replacement therapy has traditionally been prescribed in cases of male hypogonadism. This is a condition characterized by low levels of testosterone, leading to erectile dysfunction and/or a low sperm count.
What is testosterone?
As stated earlier, testosterone is the main androgen responsible for male sexuality. Physiologically, testosterone plays a crucial role in the expression of male sexual characteristics; which are:
- Primary sexual characteristics – The growth and development of the testes, penis, and other sexual organs during fetal life as well as around puberty.
- Secondary sexual characteristics – This refers to a male pattern of distribution of bodily hair including the ability to grow a beard, a deepening of the voice, improved bone density, improved muscle mass and vigor (also known as libido or sexual desire).
Notwithstanding the immense importance of the above functions, testosterone may have a very crucial role to play in fighting disease in males as well – testosterone may especially help in the treatment of metabolic conditions like obesity, cardiovascular disease (CVD) and diabetes mellitus type 2 (DM Type2).
Owing to the supposed adverse effects of testosterone therapy, physicians have always been skeptical to advocate this type of treatment. Recent research, however, tends to support the safety and effectiveness of testosterone in men with such metabolic diseases.
If indeed testosterone is as effective and safe as claimed by some researchers, does it warrant – given that the incidence of obesity (and CVD and DM Type2) has reached pandemic proportions – the use of testosterone as a health supplement on a regular basis?
The need for testosterone supplementation
Traditionally, testosterone therapy has been prescribed only to men with low blood levels of testosterone. This condition, which is medically known as hypogonadism, is associated with symptoms like erectile dysfunction, oligospermia (reduced sperm count), loss of libido and a reduced skeletal muscle mass among others.
Also, much of scientific research has tended to focus around the effectiveness of testosterone in hypogonadal men – in improving sexual functioning (Perleth, 2007), lean mass, bone mineral density and fighting osteoporosis (Wittert et al., 2003). However, the benefits of testosterone supplementation are not limited to men with low testosterone levels alone.
Testosterone use in men with normal levels of testosterone also provides benefits – the use of supplemental testosterone has been shown to reduce the incidence of osteoporosis (Anderson, Francis, & Faulkner, 1996; Kohn, 2006), fight obesity and enhance the feeling of well-being in men.
There is enough scientific basis to suggest that a reduced blood level of testosterone is inherently connected to obesity and metabolic conditions like CVD and DM Type 2 (Rodriguez et al., 2007; Mohr, Bhasin, Link, O'Donnell, & McKinlay, 2006; Kaplan, Meehan, & Shah, 2006). Furthermore, an inverse relationship seems to exist between waist circumference and testosterone levels in men (Svartberg, von, Sundsfjord, & Jorde, 2004).
What’s more, such findings seem to be consistent in men of all age groups (Svartberg et al., 2004) and from different races or ethnic backgrounds (Kupelian, Hayes, Link, Rosen, & McKinlay, 2008).
Testosterone use in older men and even in women can afford health benefits (see below).
The role of testosterone supplementation in older men
Decreased physical functioning and lack of mobility is a very realistic phenomenon in the elderly male. Much of these symptoms are caused by the normal loss of muscle mass that occurs with advancing age – a process called sarcopenia. Sarcopenia combined with the age-related decline in testosterone levels – which is even more pronounced in fat, older men (Kaplan et al., 2006) – warrants supplementation with testosterone.
Such men have been shown to benefit immensely from testosterone supplementation – the therapy improves plasma levels of testosterone (Lebrasseur et al., 2009) and in combination with physical activity has the potential to improve skeletal muscle mass and therefore physical functioning.
Testosterone supplementation in women
Not many of you would know this but androgens play important physiological roles in women as well. Not surprisingly then, an extreme androgen deficiency (especially seen in hypopituitarism or after menopause) may be detrimental to health in women (Ginzburg et al., 2010). In fact, some clinicians recommend adding testosterone to HRT (hormone replacement therapy) in post-menopausal women.
Testosterone supplementation in such women may not only improve sexual functioning, muscle mass and bone health but also psychological well-being and self-esteem.
Although this therapy was proven to be quite effective in short-term treatment regimens, much more data is still needed to prove the effectiveness and safety of testosterone on long-term use in such women (Zang & Davis, 2008).
Scientific Basis For Therapeutic Usefulness Of Testosterone Supplementation
As opposed to popular belief, numerous scientific studies hint towards the usefulness of testosterone as a therapeutic tool.
Some medical conditions which definitely warrant testosterone supplementation – either short-term or long-term are – amongst others – hypogonadism, obesity, diabetes and cardiovascular diseases.
Listed below are some medical conditions in which testosterone supplementation, as is reported by researchers, may prove to be definitely helpful. Please note that although medical literature abounds in such proofs, just a few of those studies have been cited here:
- Testosterone supplementation may offer protection from cardiovascular disease in men. In a paper published in 2010, Ginzburg and his colleagues (Ginzburg et al., 2010) showed that testosterone either alone or in combination with lipid-lowering drugs like statins causes a significant decrease in total cholesterol, low-density lipoprotein cholesterol (LDL or the ‘bad cholesterol’) and total triglycerides levels in the blood. Testosterone therapy may, therefore, translate into protection against cardiovascular disease.
- An androgen deficiency (as in hypogonadism) has been shown to be inherently connected to increased incidence of metabolic diseases (Traish, Guay, Feeley, & Saad, 2009)
- Obesity is associated with hormonal imbalances including testosterone deficiency (Seidell, Bjorntorp, Sjostrom, Kvist, & Sannerstedt, 1990). Testosterone therapy, not surprisingly, helps reduce to fat deposits in obese men.
- Androgen deprivation therapy (used for prostate cancer) causes a significant increase in body fat and decrease in lean mass (muscles and bones) (Smith, Lee, & Nathan, 2006; Smith et al., 2002; Chen et al., 2002), suggesting again that testosterone may have a role to play in improving body composition and fighting obesity
- As opposed to previous thought, low testosterone levels may be responsible for causing pancreatic cancer (von, Pina, Perez, Tavares, & Barros, 2004)
Alleged Adverse Effects of Testosterone Supplementation
Testosterone supplementation has been shown by studies to be generally safe, especially in combination with lifestyle changes – regular exercise and partaking of a wholesome, health diet (Ginzburg et al., 2010).
Some adverse effects that testosterone is believed to cause are prostate cancer, breast cancer (which can indeed affect men) and cardiovascular disease.
Testosterone and Cancer
Up until recently, a physician’s biggest fear of prescribing testosterone was the alleged risk of stimulating uncontrolled growth in the prostatic cells – leading to cancer.
Recent findings, however, tend to suggest otherwise; testosterone supplementation may not be associated with prostate cancer after all (Raynaud, 2006; Morgentaler, 2006; Raynaud, 2009). In fact, as state earlier, low levels of testosterone may increase the risk of prostatic cancer (von et al., 2004).
Use of testosterone in women (when added to hormone replacement therapy in post-menopausal women) was also thought to increase the risk of (breast) cancer. However, there is severe lack of evidence for such suggestions as well (Bitzer, Kenemans, & Mueck, 2008). Inconsistent clinical data and previously conduced, flawed trials may be to blame for such thinking on the part of physicians.
Conclusion
In a nutshell, there seems to be enough scientific evidence to suggest that testosterone supplementation* may be both effective and safe in fighting metabolic disease, improving quality of life and general well-being.
Additionally, future therapeutic will (and should), in all probability, include testosterone as an important therapeutic tool to tackle human obesity as well.
*please note that testosterone or anabolic-androgenic steroids (AAS) used for performance enhancement is sports is another topic and does not fall within the purview of this article
- Anderson, F. H., Francis, R. M., & Faulkner, K. (1996). Androgen supplementation in eugonadal men with osteoporosis-effects of 6 months of treatment on bone mineral density and cardiovascular risk factors. Bone, 18, 171-177
- Bitzer, J., Kenemans, P., & Mueck, A. O. (2008). Breast cancer risk in postmenopausal women using testosterone in combination with hormone replacement therapy. Maturitas, 59, 209-218
- Chen, Z., Maricic, M., Nguyen, P., Ahmann, F. R., Bruhn, R., & Dalkin, B. L. (2002). Low bone density and high percentage of body fat among men who were treated with androgen deprivation therapy for prostate carcinoma. Cancer, 95, 2136-2144
- Ginzburg, E., Klimas, N., Parvus, C., Life, J., Willix, R., Barber, M. J. et al. (2010). Long-term Safety of Testosterone and Growth Hormone Supplementation: A Retrospective Study of Metabolic, Cardiovascular, and Oncologic Outcomes. J Clin Med Res., 2, 159-166
- Ginzburg, E., Klimas, N., Parvus, C., Life, J., Willix, R., Barber, M. J. et al. (2010). Long-term Safety of Testosterone and Growth Hormone Supplementation: A Retrospective Study of Metabolic, Cardiovascular, and Oncologic Outcomes. J Clin Med Res., 2, 159-166
- Kaplan, S. A., Meehan, A. G., & Shah, A. (2006). The age related decrease in testosterone is significantly exacerbated in obese men with the metabolic syndrome. What are the implications for the relatively high incidence of erectile dysfunction observed in these men? J Urol, 176, 1524-1527
- Kohn, F. M. (2006). Testosterone and body functions. Aging Male, 9, 183-188
- Kupelian, V., Hayes, F. J., Link, C. L., Rosen, R., & McKinlay, J. B. (2008). Inverse association of testosterone and the metabolic syndrome in men is consistent across race and ethnic groups. J Clin Endocrinol.Metab, 93, 3403-3410
- Lebrasseur, N. K., Lajevardi, N., Miciek, R., Mazer, N., Storer, T. W., & Bhasin, S. (2009). Effects of testosterone therapy on muscle performance and physical function in older men with mobility limitations (The TOM Trial): design and methods. Contemp.Clin Trials, 30, 133-140
- Mohr, B. A., Bhasin, S., Link, C. L., O'Donnell, A. B., & McKinlay, J. B. (2006). The effect of changes in adiposity on testosterone levels in older men: longitudinal results from the Massachusetts Male Aging Study. Eur J Endocrinol., 155, 443-452
- Morgentaler, A. (2006). Testosterone replacement therapy and prostate risks: where's the beef? Can.J Urol, 13 Suppl 1, 40-43
- Perleth, M. (2007). [Testosterone--a "fountain of youth" for ageing men? Brief assessment of the efficacy and safety of androgen substitution in healthy men]. Z.Arztl.Fortbild.Qualitatssich., 101, 487-497
- Raynaud, J. P. (2006). Prostate cancer risk in testosterone-treated men. J Steroid Biochem.Mol.Biol., 102, 261-266
- Raynaud, J. P. (2009). Testosterone deficiency syndrome: treatment and cancer risk. J Steroid Biochem.Mol.Biol., 114, 96-105
- Rodriguez, A., Muller, D. C., Metter, E. J., Maggio, M., Harman, S. M., Blackman, M. R. et al. (2007). Aging, androgens, and the metabolic syndrome in a longitudinal study of aging. J Clin Endocrinol.Metab, 92, 3568-3572
- Seidell, J. C., Bjorntorp, P., Sjostrom, L., Kvist, H., & Sannerstedt, R. (1990). Visceral fat accumulation in men is positively associated with insulin, glucose, and C-peptide levels, but negatively with testosterone levels. Metabolism, 39, 897-901
- Smith, M. R., Finkelstein, J. S., McGovern, F. J., Zietman, A. L., Fallon, M. A., Schoenfeld, D. A. et al. (2002). Changes in body composition during androgen deprivation therapy for prostate cancer. J Clin Endocrinol.Metab, 87, 599-603
- Smith, M. R., Lee, H., & Nathan, D. M. (2006). Insulin sensitivity during combined androgen blockade for prostate cancer. J Clin Endocrinol.Metab, 91, 1305-1308
- Svartberg, J., von, M. D., Sundsfjord, J., & Jorde, R. (2004). Waist circumference and testosterone levels in community dwelling men. The Tromso study. Eur J Epidemiol., 19, 657-663
- Traish, A. M., Guay, A., Feeley, R., & Saad, F. (2009). The dark side of testosterone deficiency: I. Metabolic syndrome and erectile dysfunction. J Androl, 30, 10-22
- von, H. P., Pina, F., Perez, A., Tavares, M., & Barros, H. (2004). Visceral fat accumulation as a risk factor for prostate cancer. Obes Res., 12, 1930-1935
- Wittert, G. A., Chapman, I. M., Haren, M. T., Mackintosh, S., Coates, P., & Morley, J. E. (2003). Oral testosterone supplementation increases muscle and decreases fat mass in healthy elderly males with low-normal gonadal status. J Gerontol.A Biol.Sci.Med Sci., 58, 618-625
- Zang, H. & Davis, S. R. (2008). Androgen replacement therapy in androgen-deficient women with hypopituitarism. Drugs, 68, 2085-2093
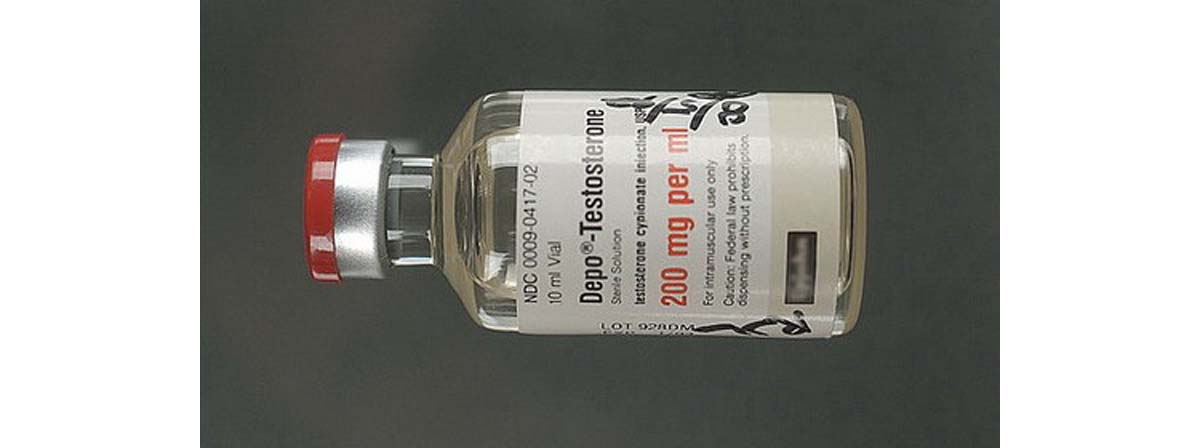
- Photo courtesy of Mark Probst by Flickr : www.flickr.com/photos/schani/14508174/
- Photo courtesy of Schlonz by Wikimedia Commons : commons.wikimedia.org/wiki/File:Depo-testosterone_200_mg_ml.jpg

