Overview
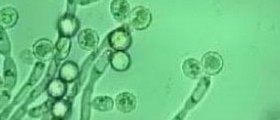
Candida glabrata was, until the late 1990s, thought to be a non-pathogenic fungal organism, but with the constant and persistent use of immune-suppressing medications, broad-spectrum antibiotics, and with the increased population of immune compromised individuals due to illnesses such as HIV, trends have shown that C. glabrata has become an opportunistic pathogenic organism of the urinary and genital tract, as well as of the bloodstream.

How the diagnosis is made
The diagnosis of C. glabrata is usually made on the culture of the specimen that was collected, which can be urine or a swab of a discharge from the vagina, for example. The culture may take up to seven days to grow, but once the specific yeast species has been isolated the identification of the organism is performed quickly.
Together with the analysis of what organism is cultured, the laboratory will also perform the appropriate tests to determine which antimycotic medications will be able to manage the organism.
A technologically advanced diagnostic tool that seems to be a promising investigation is the T2 Candida Panel which can identify Candida species such as glabrata, candida, parapsilosis, kruzei, and tropicalis directly from a blood sample without having to perform a blood culture investigation which can take many days to give a result.
Drug resistance
C. glabrata is the second most problematic and potent of the fungal infections, after Candida albicans, and medications used to manage these conditions are becoming less effective against it because of resistance against commonly used drugs such as fluconazole.
Treatment
As mentioned, there seems to be a resistance of C. glabrata against the azole antifungal medications such as ketoconazole and fluconazole, with 15 to 20 percent of cases not being affected by the medications.
C. glabrata does seem to be vulnerable to medications such as nystatin, caspofungin, flucytosine, and amphotericin B. It should be noted though that intravenous administration of the latter-mentioned drug is performed as a last resort treatment since it can cause side-effects such as chronic renal failure.
C. glabrata can also be managed with the use of a medication called terconazole in a cream based treatment for seven days. Since the infection can be persistent, and also due to its low cure rate of 40 percent, several courses of this cream may be required before the infection resolves.
Boric acid vaginal suppositories can be produced by pharmacies which can supply the patient with this product. For the management of irritation or burning of the urogenital tract, vitamin E oil is suggested as a soothing remedy for these issues.
For chronic C. glabrata infections that affect the skin or the scalp, boric acid can be used to help manage these problematic conditions.