Table of Contents
Nearly all women experience a vaginal yeast infection at least once in their lifetimes. It is estimated, however, that more than five percent of women are regularly troubled by recurring vaginal yeast infections.
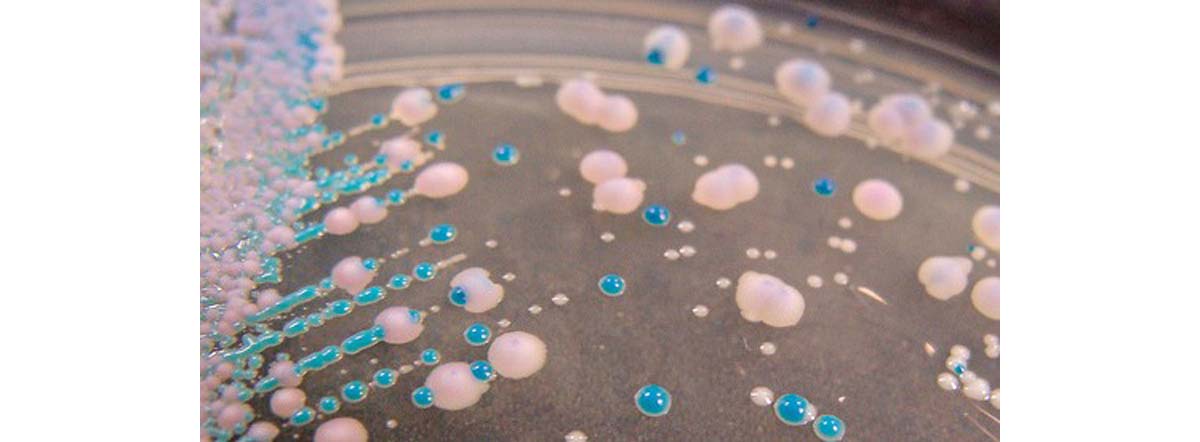
Recurring yeast infections can be defined as four or more episodes, unrelated to antibiotic treatment (more about that later) in one year. Yeasts are a type of fungus and the one most commonly responsible for vaginal infections is called Candida albicans. It is normally present in the vagina and does not usually cause any problems, as it is kept under control by other micro-organisms such as the "friendly" bacteria we depend on.
What are the symptoms of a yeast infection?
Each woman’s experience of a yeast infection may differ. The most common symptoms of a vaginal yeast infection are:
- Intense itchiness
- Soreness
- Burning and irritation of the vagina and external genital area (the vulva).
There may be redness and swelling of the area, as well as pain on urination, and during sex. Not everyone has the white ‘curd-like’ discharge traditionally thought to indicate a yeast infection. The condition is not normally associated with a bad-smelling discharge – this can indicate other infections and needs investigation by a doctor.
What causes an overgrowth of yeast?
Unfortunately there is a long list of likely candidates and in the case of recurring vaginal yeast infections it may be the same, or different factors, each time. The most common culprits are:
Ill health — if you are stressed, generally run- down, or have conditions such as diabetes, or HIV/AIDS, then you are more at risk of yeast infections. This is because your own immune system which helps to keep yeasts in check and prevents overgrowth, may be weakened, reducing its ability to do its normal job.
Medications — there is a link between some medications, particularly antibiotics, and yeast infections. This is because antibiotics, especially those effective against a wide range of bacteria (‘broad spectrum antibiotics’) upset the balance of organisms in the vagina, wiping out the bacteria which normally prevent yeasts from multiplying, due to their effect of killing the good bacteria along with the bad. Medication affecting the immune system such as steroids, or those taken following organ transplant, or to treat auto-immune diseases, can also be linked with yeast overgrowth.
This is why pregnant women and those taking high dose estrogen contraceptive pills are more susceptible to recurring yeast infections. Some women are troubled by yeast infections at particular times in the menstrual cycle, because of the connection with estrogen.
Clothing— tight or ‘sweaty’ (synthetic) underwear or clothing, and staying in wet swimwear too long may encourage overgrowth of yeasts by creating a damp and warm environment.
Douching may disrupt the balance of organisms in the vagina, leading to yeast overgrowth. The vagina is an amazing self-cleansing organ, and there is no need to use vaginal douches to keep it clean. Douching causes more harm than good.
What is used to treat yeast infections?
Creams, ointments and pessaries (solid dose forms inserted into the vagina) containing the anti-fungal fluconazole, are available to buy without a prescription. These over the counter medications work well against infections caused by Candida albicans. Doctors have a range of other anti-fungal treatments, including tablets, which they can prescribe.
- The V Book: www.thevbook.com/chapter10.html
- www.women.webmd.com/recurrent-vaginal-yeast-infections
- Photo courtesy of anshu_si on Flickr: www.flickr.com/photos/anshu_si/3989555762
- Photo courtesy of nathanreading on Flickr: www.flickr.com/photos/nathanreading/8333684249
- www.womenshealth.gov/publications/our-publications/fact-sheet/vaginal-yeast-infections.cfm

