Chemotherapy, and for purposes of keeping the conversation simple, let's use the term to refer to cancer chemotherapy, can have profound effects on the immune system. Changes in the immune system also change the way doctors can manage Lyme disease. Here's a real-world example of just how complicated making treatment decisions can be when people have both cancer and Lyme disease:
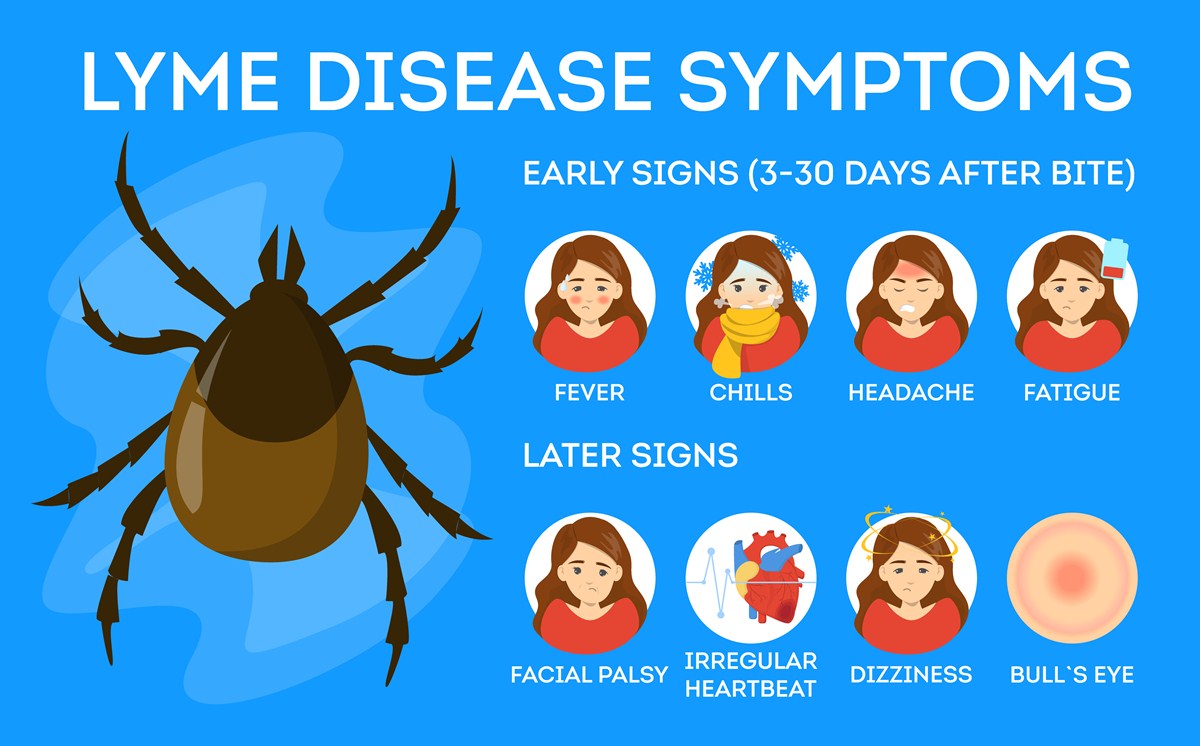
A 66-year-old woman went to see her doctor with symptoms of severe shooting pains in her legs and back, progressive loss of hearing, headaches, and weight loss. These are not unusual as symptoms of a complication of Lyme disease called neuroborreliosis, but she did not remember ever getting bitten by a tick. (Doctors look for two sets of symptoms, cranial neuropathy, which manifests itself mostly as hearing loss, and meningoradiculitis, which manifests itself mostly as headache and shooting pains.)These are somewhat more unusual as complications of lymphoma, for which she had been previously treated with chemotherapy. Lyme disease is bad, but the return of cancer is worse, so the doctor ordered tests to figure out which of two bad alternatives was causing the problem.
The first thing the doctor did was to run a simple blood test for antigens to Borrelia burgdorferi, the microorganism that causes Lyme disease. These came back negative, so the doctor did a spinal tap to take a sample of fluid to see if maybe the germ was only present in the woman's central nervous system. This result also came back negative, so the doctor ran tests for cancer. These were also negative. The patient did not have cancer, either, but the symptoms had to be caused by something.
Then the doctor sent the woman to see an infectious disease specialist, who took more blood samples and incubated them in the lab. After a few days, the microbiologist could find the actual Lyme disease organism in her blood, but her immune system, weakened by chemotherapy, could not respond to the germ and so didn't make antibodies. An immune system weakened by chemotherapy allowed the Lyme disease infection to "skip" initial symptoms (bullseye rash, flu-like symptoms, and so on) and go straight, at least from the patient's point of view, to neurological complications. Once the infection was finally treated, it could be treated an antibiotic called ceftriaxone and she got much better fast.
Lyme disease caught after chemotherapy can be seronegative, not forming antibodies because the immune system is weak. That doesn't mean that it isn't there, just that it's hard to detect. There are differences between strains of Lyme disease in Europe and North America. The germ in Europe is just a little different. It almost always causes a spike in white blood cell count before there are neurological symptoms like the shooting pains and deafness previously described. However, the whole objective of chemotherapy for lymphoma is to prevent spikes in white blood cell counts, so in some cancer patients (not just for lymphoma) this symptom won't occur, and the infection won't produce any convenient diagnostic antibodies, either.
What about using chemotherapy as a treatment for Lyme disease? The important thing to understand is that cancer chemotherapy does not treat Lyme disease. It just makes the disease more difficult to detect because the immune system is weaker. If someone who previously had Lyme disease and goes on chemotherapy fails to show antibodies in blood tests for Lyme after chemo, that doesn't mean chemotherapy cured the Lyme disease. It just means that chemotherapy weakened the immune system. Fortunately, cancer chemotherapy doesn't interfere with treatment for Lyme disease (usually). The condition will still respond to appropriate antibiotic treatment.
- van Dop WA, Kersten MJ, de Wever B, Hovius JW. Seronegative lyme neuroborreliosis in a patient using rituximab.BMJ Case Rep. 2013 Feb 14,2013. pii: bcr2012007627. doi: 10.1136/bcr-2012-007627. PMID: 23417373.
- Photo courtesy of SteadyHealth