Definition
Primary dysmenorrhea is defined by recurrent, crampy lower abdominal pain that occurs during menstruation in the absence of any other disease. Other symptoms can include nausea, vomiting, diarrhea, headache, dizziness, or back pain.
Background
For dysmenorrhea to occur, the menstrual cycles have to be established. Almost half of all female teens have ovulatory cycles two years after their menstruation has started, while two-thirds ovulate after two to four years, and 80 percent by four to five years. Ovulatory cycles mean that the girl has fully functional ovaries with menstruation.
In adolescents, 60 to 93 per cent could be having dysmenorrhea. But only 15 per cent seek medical help, which stresses the fact that doctors should be asking all females whether they have painful menstruation.

Mechanism
Dysmenorrhea is caused by altered concentrations of prostaglandins in the uterus. Prostaglandins are the chemicals responsible for normal functioning.
History
You should be prepared with this list before you visit your doctor.
1. Age when your menstruation started.
2. Duration of cycles.
3. Inter-menstrual gap.
4. Date of last two menstrual periods.
5. Relationship of cramps to bleeding.
6. Whether or not nausea, vomiting, diarrhea, back pain, dizziness, or headache occur during menstruation.
7. How severe the symptoms are (ie, how does it impact daily life).
8. What medicines you have used and what relief you got.
9. Sexual history -- type of contraception, history of sexually transmitted diseases, and history of pelvic inflammatory disease.
When we say primary, we mean that there is no known cause. Secondary, means that the pain is because of some other underlying disease.
-
Painful menses which started along with your first menstruation is unlikely to be primary dysmenorrhea. If you have pelvic pain which is unrelated to menstruation, this could be a situation where the dysmenorrhea is secondary to some other cause.
-
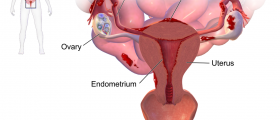
If the pain has become progressively worse over time it could be a sign of endometriosis, which may present as cyclic or noncyclic pain. Endometriosis is the presence of uterine cells in abnormal locations like the intestines and which, surprisingly, bleed like menstruation.
-
If there is a history of pelvic infection (chlymadia or gonorrhea), the adhesions resulting from the scar could be a source of pelvic pain.
Your doctor should conduct a pelvic exam to exclude the causes of secondary dysmenorrhea in all females with significant symptoms.
An internal pelvic examination may not be done in young, nonsexually active adolescents with only mild menstrual cramps.
Treatment
Treatment is decided by severity of symptoms and limitations of activities. For adolescents, nonsteroidal antiinflammatory drugs (NSAIDs) and combination estrogen-progestin contraceptives are used.Ibuprofen and naproxen are used commonly for the treatment of dysmenorrhea in clinical practice.For those who also want contraception, or for those who do not respond to or do not tolerate NSAIDs, oral contraceptive pills should be used(Please consult your doctor for this).
- Andersch B, Milsom I. An epidemiologic study of young women with dysmenorrhea. Am J Obstet Gynecol 1982,144:655.
- Hertweck SP. Dysfunctional uterine bleeding. Obstet Gynecol Clin North Am 1992,19:129
- Klein JR, Litt IF. Epidemiology of adolescent dysmenorrhea. Pediatrics 1981,68:661.
- Photo courtesy of SteadyHealth