
What Is Ulcerative Colitis?
Ulcerative colitis is a chronic and autoimmune inflammatory disease characterized by persistent and episodic ulcers that target the digestive tract. Like it's name suggests, "ulcerative colitis", the ulcers affect the colon. The disease manifests itself as painful episodes of bloody diarrhea and localized pain in the area. Furthermore, ulcerative colitis is a systemic disease, which means that although the primary target is the colon, there are some other symptoms that manifest outside of the colon, which include ulcers in the mouth, eye irritation, diffuse joint pain, skin lesions, etc. Ulcerative colitis is quite prevalent in the USA (20 cases per 100 000), and unfortunately the symptoms almost always require medical intervention for remission.

Where Does The Abdominal Pain Come From?
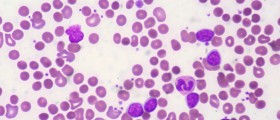
The first symptoms of ulcerative colitis are diffuse abdominal pain and bloody diarrhea. During the episodes, there is a profuse inflammatory reaction that happens in the colonic epithelium. The body's immune system is attacking the colonic mucosa, and with the combined action of colonic bacteria ketone bodies are produced, which irritate the colonic mucosa. Henceforth, the patient experiences abdominal pain. Additionally, the patient might experience what is called tenesmus, a physiological state characterized by a constant feeling of a need to empty one's bowel despite the absence of feces. This is usually observed in mild to moderate disease, but can be more pronounced if the condition becomes severe.
- Important notification about information and brand names used in this slideshow!
- Photo courtesy of Medical Center 1- Plovdiv by Picasa : lh3.googleusercontent.com/-sxv7qhxDgwo/UYzc9DEOm9I/AAAAAAAAAv0/FsW9LkxV_So/s849/colitis.jpg

Noticeable Weight Loss
With ulcerative colitis, weight loss happens through two mechanisms: first of all, increased fluids and nutrients loss. This is caused by the persistent episodes of diarrhea during which tremendous amounts of fluids are lost. Secondly, the ulcerative colitis sufferer can lose weight because of his decreased intake of food. In fact, with all gastrointestinal conditions patients generally tend to avoid eating anything, by fear of possibly worsening the condition. In addition to this, their appetite is generally decreased, anyways. Even in hospital settings, Doctors avoid feeding patients orally (nil per os) when they suspect a gastrointestinal condition, and patients are almost always fed through IV.
- Important notification about information and brand names used in this slideshow!
- Photo courtesy of Daniel Oines by Flickr : www.flickr.com/photos/dno1967b/8040604426/

Commonly Used Medications For The Management Of Ulcerative Colitis
As previously mentioned, anti-inflammatory are the first line of medications used in the management of ulcerative colitis. Aminosalicyclates (Sulfasalazine, Mesalazine, Balsalazide, Olsalazine, etc.) are ideal, because they work both as an ainti-inflammatory and anti-bacterial. When they are broken down in the intestines, their active ingredient, 5-aminosalicylic acid (5-ASA) works to monitor the inflammation. They also have an anti-oxidant action that allows them to fight bacteria and protect the colonic epithelium from undergoing more damage. Steroids (prednisone, cortisone, etc.) are also given to reinforce the anti-inflammatory effect. Hydrocortisone is applied topically for the skin lesions. Additionally, immunosuppresive drugs (such as azathioprine, mercaptopurine) are given to lessen the immune system's response.
- Important notification about information and brand names used in this slideshow!
- Photo courtesy of Paul Huxley by Flickr : www.flickr.com/photos/9139977@N05/6104448615/

Skin Sores
Alongside with the Crohn’s disease, the other inflammatory bowel disease of that type; ulcerative colitis presents with a wide variety of skin lesions. The most common, Erythema Nodosum – which literally means “red bumps” – appears either just before or during the flare-ups and is most commonly seen over the shins, the ankles and the arms. It tends to regress when the symptoms are managed. Next to that, there is Pyoderma Gangrenosum, which are deep ulcers filled with pus and present at the surface of the skin. Initially, the Pyoderma Gangrenosum lesions start as small blisters, but eventually end up joining to form deeper ulcers. Enterocutaneous fistulas may also develop and form a bridging gap between the colon, rectum or anus, and the skin. They may also leak pus or fecal matter, depending on the situation. All these cutaneous ulcers tend to regress when the disease is better managed. However, topical ointments, antibacterial and anti-inflammatory creams can be applied.

Who Gets Ulcerative Colitis?
This is rather an interesting yet intriguing question. 20% of cases of ulcerative colitis are hereditary, and those who develop the disease are very likely to have a first-degree relative (father, mother, sister or brother) with the symptoms of the disease. Additionally, ulcerative colitis is more prevalent in people of Jewish decent (2 or 4 times higher) compared to other racial groups. It is also more commonly observed in white people, compared to African Americans. Regarding gender, ulcerative colitis is more likely to occur in women than men, following the pattern of the majority of auto-immune diseases. Lastly, ulcerative colitis is more common in developed countries (USA, northern Europe) than in developing countries.

Urgent Care
In the management of ulcerative colitis, the protocols involve treating the acute symptoms first, then managing a potential relapse. Aminosalicyclates, which are anti-inflammatory drugs are used in a hospital setting as the first line treatment option for the management of a ulcerative colitis flare-up. They help in relieving the inflammation, thus attenuating the majority of the symptoms. Corticosteroids are also used in the urgent care setting, and they have a symbiotic effect on the inflammation. Because dehydration and electrolyte imbalance might have occured following the persistent diarrhea, the patient can be put under IV for fluid restoration. Finally, the patient should be restricted to a "nil per os" regimen.
- Important notification about information and brand names used in this slideshow!
- Photo courtesy of DIBP images by Flickr : www.flickr.com/photos/diacimages/5774906354

What Can Cause Ulcerative Colitis?
Ulcerative Colitis is a genetic disease, transmitted from generations to generations. That means both good news and bad news: for those who have a family history of ulcerative colitis, they are very likely to develop it; whereas those who do not have a family history of ulcerative colitis are not at risk. However, having a family history of this inflammatory bowel disease doesn't automatically mean that you will develop the disease. In fact, there are some environmental factors that play a role in disease development, and the most important one is the diet. Diets rich in unsaturated fats and poor in dietary fibers were proven to play a role in triggering ulcerative colitis in at-risk patients. In addition, physical and emotional stress could also be implicated in inflammatory outbreaks.
- Important notification about information and brand names used in this slideshow!
- Photo courtesy of Juli by Flickr : www.flickr.com/photos/julishannon/5530622078/

Ulcerative Colitis In Children
It can be very scary to see your child experiencing recurrent episodes of abdominal pain, cramps and diarrhea. The good thing is, once the disease is diagnosed, treatment can be initiated and children are known for responding quite well to ulcerative colitis treatment. While managing ulcerative colitis in children, several factors need to be included: medications, diet and lifestyle adjustments, nutritional counseling, surgical care (if necessary) and most importantly, psychological support. Needless to say, a chronic and life-changing disease as this one could cause some level of psychological trauma as your child will need to make a lot of sacrifices and possibly abstain from the things he/she loves eating the most. Therefore, parental support is crucial to make the child more accepting of his condition, and allow him/her to live a normal life with ulcerative colitis.

Alternative Treatment: Biological Therapies
Next to the commonly used medications for the treatment of ulcerative colitis, there are also some herbal medicines and natural remedies that have been reported effective in the management of ulcerative colitis flare-ups. First of all, we have the commonly encountered fish oil. Fish oil provides a chemical called Eicosapentaenoic acid (EPA); that belong to the class of eicosanoids. EPA inhibits the activity of leukotrienes, chemical mediators involved in inflammation. We can also name Boswellia, an Indian Ayurvedic herb that is used in inflammatory conditions because of its boswellic acids. In Africa, it has already been reported that a species of Boswellia, Boswellia dalzielii; was used to treat rheumatism and gastrointestinal problems. Lastly, medical cannabis can be used to reduce the abdominal discomfort that is experienced during ulcerative colitis flare-ups.
- Important notification about information and brand names used in this slideshow!
- Photo courtesy of New Media Ba by Picasa : lh4.googleusercontent.com/-5PT6qtViIF4/TYciJdBnlnI/AAAAAAAAHwo/PjDPJQEpK08/s1152/infuzija.jpg
- source 1: en.wikipedia.org/wiki/Boswellia#Medicinal_uses
- source 2: en.wikipedia.org/wiki/Management_of_ulcerative_colitis























Your thoughts on this
Loading...