Bone mineral density (BMD) testing is the clinical gold standard for determining future fracture risk by measuring bone mineral loss. If your bone mineral density is low, you have elevated risk of breaking a bone.
Any bone in your body can break. The most vulnerable bones in your body are the hip bones, ribs, wrists, forearms, and spinal vertebrae. When bone mineral density is exceptionally low, it doesn't take much trauma to break a bone. You might fracture a vertebra by pulling a car door shut. You might break a rib by laughing or sneezing. Knowing your bone mineral density gives you a vital warning that you need to start working with your doctor for better bone health right away.
Dual-Energy X-Ray Absorptiometry (DXA)
When you have a dual-energy X-ray absorptiometry (DXA) test for bone mineral loss, you lay on a table as a machine hums, moving back and forth over you. Inside the table beneath you, a very small amount of electromagnetic is generated. As the X-ray beam passed through your body, some of it was weakened or blocked by the mineral content of your bones. The scanner above your body measures the energy that was not blocked. The more minerals that are present in your bones, the more radiation is blocked. The machine calculated your bone mineral content in grams for a specific area of bone. Then to compare your bone mineral density to standards for bone mineral density, this information is converted into T and Z scores.
Two readings of bone mineral density on your DXA scan report
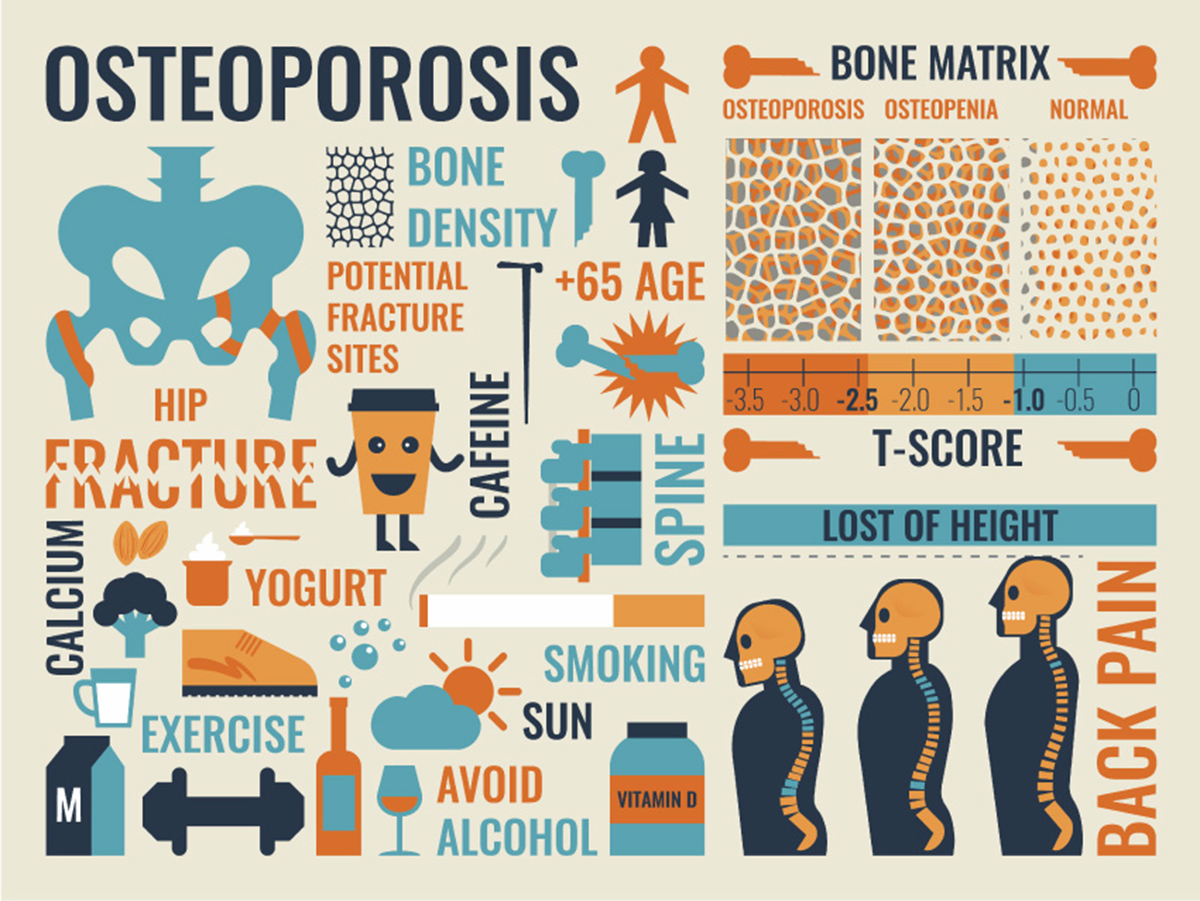
Those of you who are familiar with statistics know that t and z are two different statistics for measurements of different sizes of samples. In a DXA scan, the T score compares your bone mineral density to that of a healthy young woman. The Z score compares your bone mineral density to that of people of your sex and age. Osteoporosis is defined as any bone density T score that is more that 2.5 standard deviations below that of a white, healthy, young woman.
It isn't necessary to have exactly the same T score of zero or higher (the same bone mineral density as this theoretical white, healthy, young woman or better) to avoid being labeled with osteoporosis. Normal bone mineral density is any T score greater than or equal to -1.0. (If your bone mineral density scan falls within 1 standard deviation of this model woman, even if it is lower, you are still considered to have normal bone mineral density.) Low bone mass or osteopenia is defined with a T score between -2.5 and -1.0, and severe or established osteoporosis is defined by any T score of -2.5 or lower.
No magic numbers in bone densitometry testing
There is no magic number that definitively describes your risk of breaking a bone. Someone who has osteopenia and a T score of -2.45 is about as likely to endure a fracture as someone who has osteoporosis and a T score of -2.55. But for every standard deviation of your T score goes below zero, you risk of fracture doubles.
One clinic may diagnose you with osteopenia and another clinic may diagnose you with osteoporosis even though your bone mineral density has not changed. That is because there are slight differences with different machines and different radiologists. Changes in T scores are most meaningful when they are the results of testing with the same equipment interpreted by the same radiologist. Bone mineral density may also change with the seasons. If you get a lot of sun in the summer, or if you don't, the fluctuations in your vitamin D levels may be be reflected in changes in your T scores.
Generally, your doctor will discount any change in your T score that is less than 3 percent, chalking it up to changes in testing or changes in temporary lifestyle factors. If your T score falls from -3.05 to -3.10, the doctor won't say that you're worse. Or if the your score rises from -2.50 to -2.45, the doctor won't say that you're better.
DXA scans are very safe
There is no reason to worry about the amount of radiation you receive in a DXA scan. A central scan (looking at hip and spine) exposes you to between 1 and 5 sieverts of radiation. In comparison, a lumbar spine x-ray exposes you to 700 sieverts. A mammogram generates 450 sieverts. Just remaining on the surface of the earth exposes you to 5 to 8 sieverts of radiation.
But the DXA scan T score is not the last word on your bone health
DXA scanning isn't enough to give you a clean bill of health. When you have a DXA scan, you also need to be assessed for spinal compression fractures. These tiny breaks in the vertebrae may not hurt, but it is important to identify them. (A good sign that you have spinal compression fractures is loss of height.) A confirmed spinal compression fracture requires nutritional intervention and medication, no matter what your T score is. To check for compression fractures, your doctor will order with a vertebral fracture assessment (VFA), which done on the same machine as DXA, or spinal X-rays.
- F. Cosman, S. J. de Beur, M. S. LeBoff, E. M. Lewiecki, B. Tanner, S. Randall, R. Lindsay. Clinician’s Guide to Prevention and Treatment of Osteoporosis.Osteoporos Int. 2014. 25(10): 2359–2381. Published online 2014 Aug 15. doi: 10.1007/s00198-014-2794-2. Correction in: Osteoporos Int. 2015
- 26(7): 2045–2047. PMCID: PMC4176573.
- J. A. Kanis, E. V. McCloskey, H. Johansson, C. Cooper, R. Rizzoli, J.-Y. Reginster, on behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013. 24(1): 23–57. Published online 2012 Oct 19. doi: 10.1007/s00198-012-2074-y PMCID: PMC3587294.
- Eugenia Negredo, Anna Bonjoch, Moisés Gómez-Mateu, Carla Estany, Jordi Puig, Nuria Perez-Alvarez, Joaquin Rosales, Silvana di Gregorio, Luis del Rio, Guadalupe Gómez, Bonaventura Clotet. Time of Progression to Osteopenia/Osteoporosis in Chronically HIV-Infected Patients: Screening DXA Scan. PLoS One. 2012. 7(10): e46031. Published online 2012 Oct 8. doi: 10.1371/journal.pone.0046031. PMCID: PMC3466220.
- Photo courtesy of SteadyHealth.com


Your thoughts on this