Table of Contents
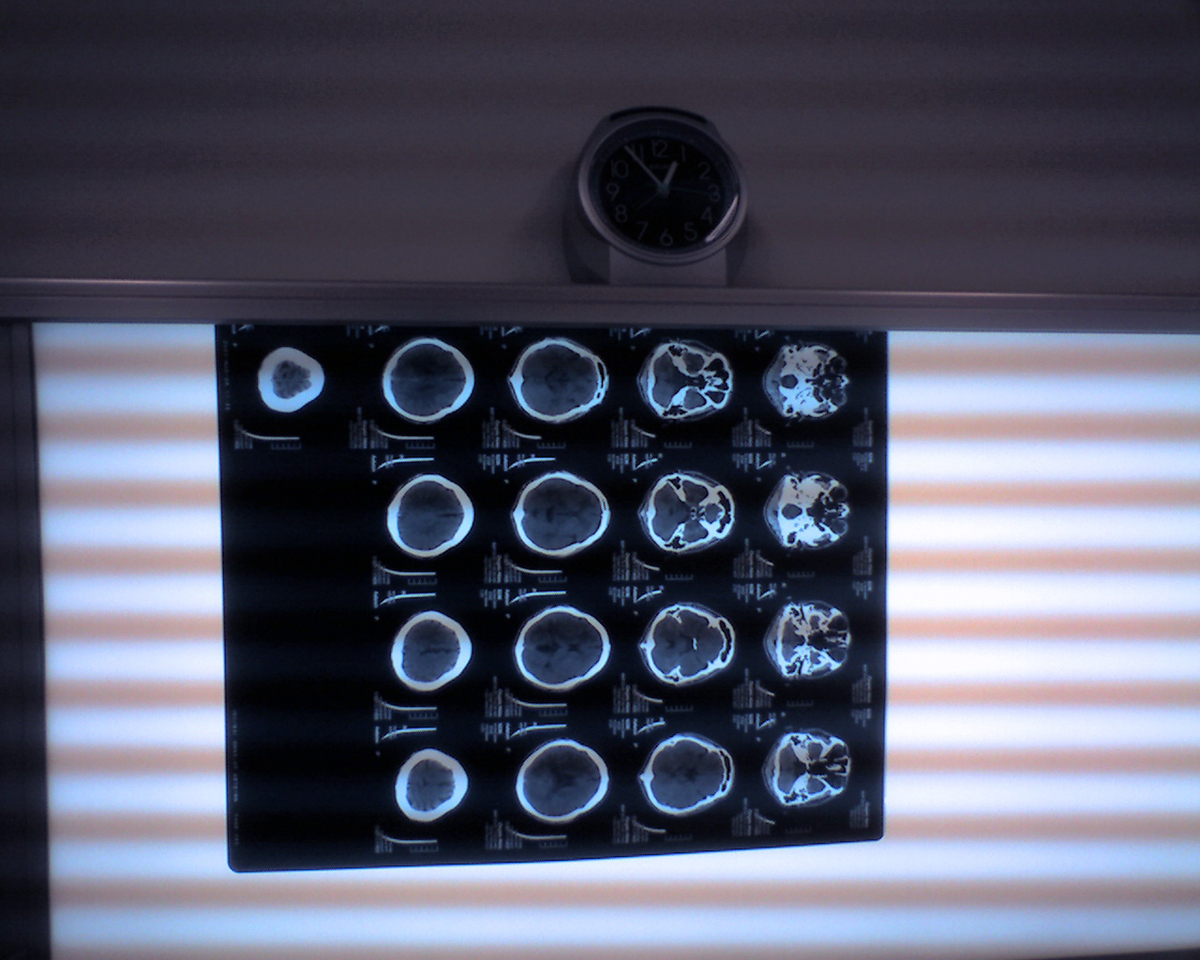
Idiopathic basal ganglia calcification is also known as Fahr’s syndrome. The disorder a highly uncommon, genetically dominant disease of neurological origins, which is characterized by abnormal calcium deposits in the portions of the brain which control movement.
Common signs and symptoms experienced with Fahr’s syndrome:
These symptoms are some of the things a person may experience with Fahr’s syndrome:
- Motor function deterioration: Involves changes in motor function or abilities.
- Dementia
- Mental retardation
- Spastic paralysis
- Dysarthria (poorly articulated speech)
- Athetosis (involuntary, writhing movements)
- Eye impairments
- Optic atrophy
- Small head
- Round head
- Extrapyramidal disorder (defects in basal ganglia functioning)
- Tremors
- Spasticity (limb stiffness)
- Muscle rigidity
- Mask-like appearance of the face
- Shuffling gait
What are some of the less common signs and symptoms of Fahr’s syndrome?
Some of the most uncommon symptoms of Fahr’s syndrome can include the following:
- Chorea (rapid, jerky, involuntary movements)
- Seizures
- Pill-rolling finger motions
- Dystonia (twisting, repetitive muscle contractions)
What is the age of onset for Fahr’s Syndrome?
The average age of onset of Fahr’s Syndrome is different for each individual. However, the disease most commonly presents in individuals around the 3rd and 4th decade of their life.
What causes Fahr’s Syndrome?
Fahr’s syndrome is most often transmitted as an autosomal dominant trait, but it can also be passed from parent to child through an autosomal recessive trait or it could occur sporadically. A locus at 14q (IBGC1) has been thought to be involved. A secondary locus has been identified on chromosome 8 and a third on chromosome 2. More study of the disease is needed in order to determine exactly what role genetics plays in the development of Fahr’s syndrome.
How is Fahr’s syndrome inherited?
A person can inherit Fahr’s syndrome as an autosomal recessive trait in which both parents are carriers of the gene.
How is Fahr’s syndrome diagnosed?
In Fahr’s syndrome, a doctor will have to investigate certain blood and biochemical factors and may perform the following tests to make a proper diagnosis:
- Natural killer cells should be assessed in suspected cases of Fahr’s syndrome, because in patients with the disease, levels will be elevated.
- Levels of urinary cAMP, osteocalcin, serum lactic acid and creatinine should be tested at resting levels and after exercising.
- Serum levels of magnesium, calcium, alkaline phosphatase, calcitonin and PTH should be tested.
- The Ellisworth Howard test should be performed, an increased level of urinary cAMP would aid in diagnosis.
- An evaluation of viruses, parasites and bacteria should be done.
See Also: Neurologial Disorders In Children
What are the diagnostic criteria for Fahr’s Syndrome?
The diagnostic criterion for Fahr’s Syndrome has changed and is stated as the following:
- Familial history which is consistent with autosomal dominant inheritance
- Bilateral calcification located within the basal ganglia through the use of neuroimaging. Other areas of the brain could also contain calcifications.
- Progressive neurological dysfunction, which generally includes movement difficulties and possibly neuropsychiatric manifestations.
- Although the average age of onset normally happens between the ages of 30-40, there are some cases of brain stones being diagnosed in children.
- Absence of biochemical abnormalities and physical features which suggest a mitochondrial, metabolic or systemic disorder
- www.ninds.nih.gov/disorders/fahrs/fahrs.htm
- www.rightdiagnosis.com/f/fahrs_syndrome/intro.htm
- www.ncbi.nlm.nih.gov/pmc/articles/PMC3616573/
- patients.aan.com/disorders/index.cfm?event=view&disorder_id=922
- radiopaedia.org/articles/fahr-disease
- medind.nic.in/jac/t10/i3/jact10i3p239.pdf
- Photo courtesy of Akira Ohgaki by Flickr: www.flickr.com/photos/akiraohgaki/427828872
- Photo courtesy of Thirteen Of Clubs by Flickr: www.flickr.com/photos/thirteenofclubs/5457976870

