Our body is a very sophisticated piece of machinery which is designed to overcome even the worst conditions. It is composed by several systems that regulate every activity that our body performs. One of these systems is the immune system, which acts as a well-organized army that keeps any harmful living or non-living thing under control, preventing our body from being damaged.
Unfortunately, as any other machine, our body can sometimes start working wrong and instead of helping us in maintaining the right balance, it can cause severe damage to its own tissues and organs. This is the case of systemic lupus erythematosus (SLE), an autoimmune disease caused by an alteration in the immune system of patients that suffer from the illness.
The immune system in a healthy person
In a normal person, the immune system reacts against microorganisms, like bacteria, viruses, fungus and parasites and other non-living particles, such as pollen or specific substances in certain foods, that could potentially harm any tissue.
Immune cells detect antigens and they immediately put in action their plan or plans of attack. This reaction involves diverse defense mechanisms, including inflammation, which main objective is to get rid of whatever is causing an alteration in the normal balance of the body functions.
When the immune system is stimulated by one or more antigens, it is active until the potential threat is eliminated; after this, the immune system returns to its normal state, patrolling all our body and ensuring everything is working properly.
The immune system going crazy
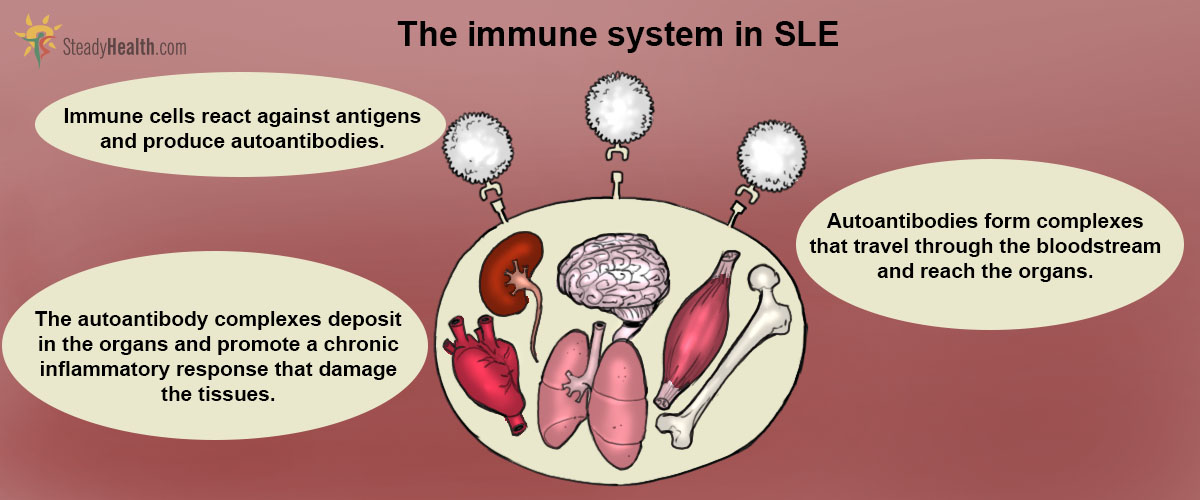
What happens in patients suffering from SLE? This disease is caused by a lack of tolerance from our immune system towards our own antigens.
One of these reactions is the production of antibodies, or in this case, autoantibodies, which are proteins that attach to the antigens in order to flag them and attract killer immune cells towards them. The production of autoantibodies is really intense, and they tend to gather and deposit in various organs, promoting the recruitment of immune cells to the site.
See Also: Lupus in Women: Chronic Inflammatory Disease
Why is this bad? Well, during inflammation, immune cells start releasing several substances, called cytokines. Some of them have the ability to recruit more immune cells to the site where the damage was detected; others are in charge of attacking the microorganisms directly. When the inflammatory response is chronic, these substances start damaging the patient’s organs where the autoantibodies deposit.
Characteristics Of Systemic Lupus Erythematosus (SLE)
SLE is not an easy illness to describe. Since the autoantibodies that the immune system produce can attack basically any organ, symptoms and signs are quite varied, and most of the times it is very difficult for doctors to diagnose a patient with this disease.

Symptomatology
Since autoantibodies target several organs, the symptomatology of the disease is not specific, so doctors have tried to classify it in various types, depending on the symptoms and the organs that are affected.
Specific symptoms are caused by autoantibodies affecting mainly the musculoskeletal, cardiac, pulmonary, renal, gastrointestinal and neurological systems. A patient with musculoskeletal SLE, for example, would experience arthralgia and arthritis, as well as muscular stiffness.
What causes SLE?
It is not quite clear why the immune system fails and attacks the patient's own antigens. This disease has been related to genetic factors, but it is also possible that hormones and environmental factors, such as UV radiation and specific viral infections, have a lot to do with the loss of immune tolerance.
SLE diagnosis relies mainly in the detection of the autoantibodies and an increase in the count of immune cells, detected in a blood test. This data, along with the evaluation of the signs and symptoms that the patient refers, help the doctor in the diagnosis of the disease.
Steroids are the most common type of immunosuppressants and are widely used, not only to treat SLE, but also to treat other autoimmune diseases. Of course, the use of steroids represents a risk, because they put the patient into a state of immunosuppression, meaning that its system is switched off and in case of an infection, it won’t be able to respond properly.
Apart from the use of immunosuppressive agents, SLE patients also take medications to control the symptoms caused by the organ damage and to prevent further consequences. For example, they are prescribed with medications to control blood pressure, to prevent and treat osteoporosis, and other agents that help in the prevention of infections, such as antibiotics.
Biologic drugs are typically reserved for individuals with moderate to severe lupus who have not responded well to other standard treatments. Belimumab is the first and only biologic drug specifically approved by the U.S. Food and Drug Administration (FDA) for the treatment of SLE. It works by targeting a protein called B-lymphocyte stimulator (BLyS) that plays a role in the overactivity of the immune system seen in lupus. Belimumab can be administered by intravenous infusion or subcutaneous injection.
See Also: Systemic lupus erythematosus (SLE)
Nowadays, thanks to an improvement in medications and diagnostic methods, patients with SLE have a better prognosis than a few years ago. Even so, their mortality rate is three times higher than that of the normal population, but hopefully, with the research that is being carried out at the moment on this illness and other similar ones, better ways to treat and improve the quality of patients will be found.
Living with lupus may require ongoing management and lifestyle adjustments, but with proper medical care and self-care, many people with lupus can lead fulfilling lives.
- MOK, C. C. & LAU, C. S. 2003. Pathogenesis of systemic lupus erythematosus. J Clin Pathol, 56, 481-90.
- Mindmap by steadyhealth.com
- Photo courtesy of Eric Schmuttenmaer by Flickr : www.flickr.com/photos/akeg/4573405885