Does too much sadness increase your risk for heart disease? Or, can depression lead to a heart attack? Although sadness is often associated with a broken heart in popular literature, the direct link between depression and development of coronary artery disease in people who were previously healthy has not been established until fairly recently.
In fact, recent studies found that chronic depression can increase your risk of developing coronary heart disease and may even lead to a heart attack. The studies also suggested that treating depression may even prevent heart disease and its complications.
Does treating depression really prevent heart disease? Is there really a link between these two conditions?
Let's take a look.
What is Depression?
Sadness is a common experience for everyone, and we all experience this emotion plenty of times in our lives. Sadness is a completely normal emotion that everyone feels. Sometimes, however, we feel more than just sadness. Everyone undergoes a feeling of depression after a major life problem or loss occurs in their life. But most people are often able to recover from feelings of sadness, loss of appetite, trouble sleeping, and other symptoms within a few days or weeks. They are able to move on and go back to their normal activities in life, even if sad thoughts sometimes do come back. We all go through tough times in our lives, and that doesn't mean that you have clinical depression.
On the other hand, some people experience deep sadness that may prevent them from leading a normal life. This may be a sign of depression.
When chronic depression interferes with one's ability to lead a normal life, mental experts refer to it as a major depressive disorder. This is a serious mental disorder that can reduce the quality of one's life. It affects about 6.7% of adults in the US and can cause other health problems.
Treatment may come in various forms, but what is important is for the individual to get help to reduce his risk for other health problems such as heart disease.
Treat Depression and Prevent Heart Disease
Previous studies linking depression with heart disease have been inconsistent. Recently, however, two new studies have shown that symptoms of major depression may increase one's risk for coronary heart disease. Major depressive disorders may also increase the likelihood that one will suffer from a heart attack.
Coronary heart disease (CHD) occurs when the blood flow to the heart muscles is reduced due to narrowing of the blood vessels (coronary arteries) supplying the heart with oxygen and nutrients. There are many factors that can cause CHD including poor diet, a sedentary lifestyle, smoking, and other health conditions. Recently, the link between chronic depression and CHD has been supported by a study that involved more than 10,000 adults in London who were followed up for a span of 24 years. The participants were evaluated up to six times during this period for depressive symptoms using a health questionaire. They were also evaluated once using the Epidemiologic Studies Depression Scale. The results showed that participants who were screened positive for depression on more than two occasions were more likely to develop heart disease than those who were not chronically depressed. In addition, the researchers also found that depressed individuals also had a higher risk of suffering from a heart attack or from dying from after a heart attack.
See Also: A New Way To Treat Depression: Scalp Electrodes
These findings have led mental health experts to conclude that treating depression may prevent people from developing CHD and from suffering from a fatal or nonfatal heart attack.
Symptoms Of Depression
To treat depression it is first important for an individual or his family, friends or healthcare giver to recognize the signs and symptoms of depression. Symptoms of depression include:

-
Persistent sadness or feelings of emptiness
-
Feelings of hopelessness
-
Feelings of guilt, anxiety, worry and helplessness
-
Restlessness and irritability
-
Constant feeling of tiredness
-
Problems with concentration, memory and decision-making
-
Changes in eating habits (either loss of appetite or overeating)
-
Trouble sleeping
-
Thought of dying or self-harm
-
Persistent headaches, body aches, and gastrointestinal symptoms that do not get better with treatment
Sometimes people dismiss these symptoms and assume that an individual will soon get over it when things get better. However, delaying diagnosis and treatment may lead to serious health consequences, including heart disease. Other people who have trouble coping with depression turn to substance abuse or even self-harm or suicide because they did not get immediate help.
It is also important to seek help when you have trouble getting help from family or friends and you feel withdrawn and isolated. If you have thoughts of suicide, call your doctor or a 24-hour suicide hotline immediately.
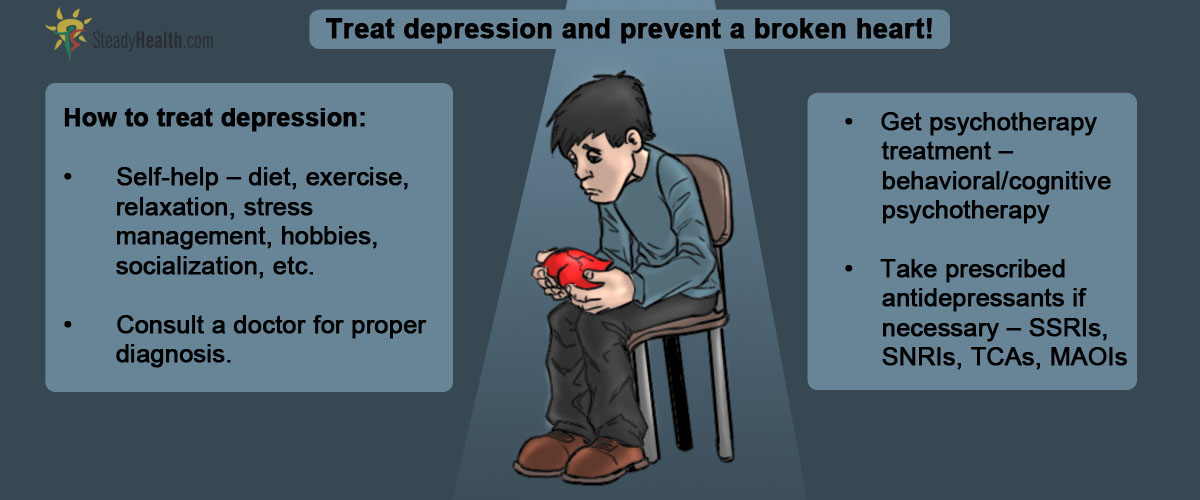
Treatments for Depression
Self-Help
People can sometimes bring themselves to cope with depressive moods by doing some self-help methods daily. These include:
-
Getting dressed daily.
-
Going out for a walk or doing other forms of exercise regularly.
-
Practicing relaxation techniques like yoga and meditation
-
Setting realistic goals and practicing stress management techniques.
-
Engaging in social activities or pursuing a hobby.
-
Sharing feeling with family, friends or religious members of the community.
-
Getting enough rest and sleep.
-
Eating a well balanced diet and avoiding overeating.
-
Attending community support groups.
-
Avoiding smoking, alcohol and drug abuse.
If these self-help methods do not improve your symptoms, seek professional help for proper diagnosis and treatment.
Psychotherapy
Your primary care physician can help you contact a mental health professional who can give proper diagnosis and treatment for depression. For mild to moderate depression psychotherapy or “talk therapy” can help reduce depressive symptoms.
There are different forms of psychotherapy and these may be done one-on-one with a trained therapist or may be done with the family or a group of individuals. These may include behavioral therapy, which focuses on learning new behaviors to modify unhealthy patterns of behavior. It may also use cognitive therapy, which emphasizes on modifying dysfunctional thinking processes that lead to unhealthy behaviors and emotions.
See Also: What depression does to a person?
Medications
For severe depression, self-help and psychotherapy may not be enough to treat one's symptoms. In addition to these treatments, physicians may need to prescribe antidepressants to help restore balance in the chemical environment in the brain. Neurotransmitters are brain chemicals that are involved in regulating mood. These chemicals include serotonin, norepinephrine, and dopamine. Imbalances in these neurotransmitters may be improved by taking certain antidepressants, such as:
-
Selective serotonin reuptake inhibitors (SSRIs) - examples: fluoxetine (Prozac), escitalopram (Lexapro), sertraline (Zoloft), paroxetine (Paxil)
-
Serotonin and norepinephrine reuptake inhibitors (SNRIs) - examples: duloxetine (Cymbalta) and venlafaxine (Effexor)
-
Bupropion (Wellbutrin)
-
Tricyclics antidepressants
-
Monoamine oxidase inhibitors (MAOIs)
These medications usually need four to six weeks of intake before significant improvements occur. They must also be taken as directed and must not be stopped when one feels better without a doctor's advice.
- Medpage Today. Treat Depression to Prevent CVD? http://www.medpagetoday.com/Cardiology/Prevention/44183
- Brunner EJ, Shipley MJ, Britton AR, et al. Depressive disorder, coronary heart disease, and stroke: dose-response and reverse causation effects in the Whitehall II cohort study. Eur J Prev Cardiol. 2014. http://cpr.sagepub.com/content/21/3/340
- J. C. Stewart, A. J. Perkins, C. M. Callahan. Effect of Collaborative Care for Depression on Risk of Cardiovascular Events: Data From the IMPACT Randomized Controlled Trial. Psychosomatic Medicine, 2013
- 76. http://www.psychosomaticmedicine.org/content/76/1/29.abstract?sid=75e7f5ee-c390-4635-bc7b-07a17f1b1c38
- NIH. Depression. http://www.nimh.nih.gov/health/publications/depression/index.shtml#pub6
- Mindmap by steadyhealth.com
- Photo courtesy of Johanna Hardell by Flickr : www.flickr.com/photos/34328559@N03/3255592441
- www.medpagetoday.com
- cpr.sagepub.com
- www.psychosomaticmedicine.org
- www.nimh.nih.gov/health


Your thoughts on this