What is ulcerative colitis?
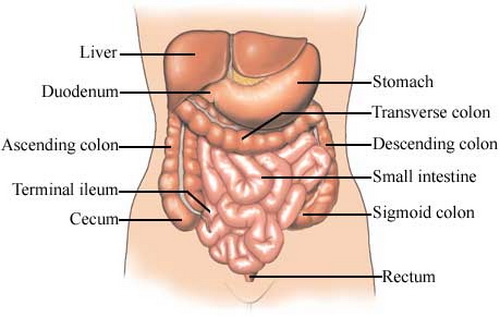
Ulcerative colitis is a type of inflammatory bowel disease affecting the cells which form the mucosal lining of the colon and the rectum. There is ulceration of these parts of the gut which may cause bleeding, pus discharge, diarrhea and pain in lower abdomen. Large intestine is the part of the gastrointestinal tract which is responsible for the absorption of water from the stools and the transformation of the stools from liquid to solid state. However, because of ulcerations in the large intestine, water is not absorbed properly leading to frequent episodes of diarrhea. The disease usually begins during adolescence between the ages of 15 and 25, but there is another small peak between the ages of 55 and 65. Both men and women are affected equally.

Warning signs of ulcerative colitis
Some of the early symptoms which should set the alarm bells ringing for the possibility of ulcerative colitis include: • Pain in lower abdomen: It is one of the commonest symptoms of ulcerative colitis. It is caused due to inflammation of the colon and rectum. The pain may vary in frequency and intensity from patient to patient. • Diarrhea/ blood in stools: As water cannot be absorbed properly from the lower gut because of the disease, the patient often suffers from diarrhea. Ulcers in the colon and rectum may bleed which leads to the presence of blood in the stools. • Weight loss: Inflammation of the gut can lead to digestive problems. As a result, the patient may notice persistent weight loss, reduced appetite and nausea. • Other warning signs: Other signs may include joint pains, anemia, lethargy, fever and skin sores.

Who is at risk of developing ulcerative colitis?
Ulcerative colitis is a common disease condition in developed countries but its incidence is remarkably low in the developing and under-developed countries. In developed countries, the white population is more prone to suffer from this condition. People of Caucasian and Jewish descent are more likely to develop ulcerative colitis. Ulcerative colitis has a genetic predisposition. A person is at high risk of developing the disease if a close family member or a first degree relative is already a patient of this disease. Adolescents and young adults between the ages of 15 and 25 are at the highest risk. However, a small risk is also present for people in between the ages of 55 and 65. Ulcerative colitis affects both men and women equally.
- Important notification about information and brand names used in this slideshow!
- Photo courtesy of Kevin Dooley by Flickr : www.flickr.com/photos/pagedooley/7710386996/
What causes ulcerative colitis?
Although the exact cause of ulcerative cause has still not been found, many experts believe that the condition results because of abnormal activation of the body’s immune system. A normal human gut is colonized with millions of bacteria. These bacteria constitute the natural flora and help in building up the body’s immunity. However, scientists say that in patients with ulcerative colitis, the body’s immune cells start acting against these naturally occurring bacteria. Apart from killing these friendly bacteria, the disease process also kills the cells forming the mucosal lining of the gut leading to symptoms of ulcerative colitis. Another school of thought is that ulcerative colitis is caused by genetic abnormalities. Supporters of this theory, point out that the disease tends to run in families, and is often seen in close relatives. Ulcerative colitis is said to be triggered by emotional stress and sensitivity to certain food products.
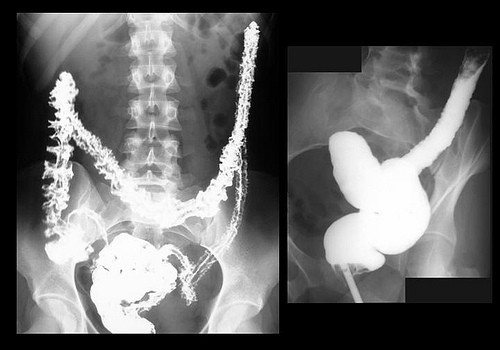
How is ulcerative colitis diagnosed?
Several diagnostic tests are employed to diagnose ulcerative colitis. These include: • Colonoscopy: This is the most definitive method of diagnosing ulcerative colitis. An endoscope is introduced through the rectum and the interiors of the rectum and colon are examined. Inflammation and ulceration of the mucosal lining of these parts of the gut help in diagnosing the condition as ulcerative colitis. It can also help in differentiating the condition from Crohn’s disease, diverticulitis and colon cancer. Biopsy from suspected areas can be taken to further confirm the diagnosis. • Stool examination: The patient’s stool is examined to see the presence of blood and pus. It is also useful in ruling out conditions like parasitic infestation which may mimic the symptoms of ulcerative colitis. A protein, calprotectin, when present in stools, is an early biomarker of inflammatory bowel disease, when other symptoms of the disease have not become so marked. • Blood tests: Blood of the patient can be examined for the presence of anemia, a raises white blood cell count and a raised ESR. The latter two show the presence of an ongoing inflammatory process.

When is hospitalization necessary in patients with ulcerative colitis?
There are several complications of ulcerative colitis in which the patient requires urgent hospitalization and expert care. These conditions include: • An ulcer that is bleeding excessively. • Excessive diarrhea which may lead to dehydration. • Sudden tear in the colon which may require surgical intervention. • Development of toxic megacolon which does not respond to medical treatment. The patient is admitted for surgical intervention in such cases. • A fulminant attack of ulcerative colitis not responding to medications may require immediate surgery. Based on the severity of the symptoms, ulcerative colitis can be graded as follows: • Mild: There are fewer than 4 episodes of bleeding per rectum per day. • Moderate: There are more than four episodes of bleeding per rectum per day. • Severe: There are more than four episodes of bleeding per rectum per day and there is presence of systemic illness and hypoalbuminemia (< 30 g/dL).

Complications of ulcerative colitis including colon cancer
One of the most feared complications of ulcerative colitis is colon cancer. Estimates tell us that almost 5% of patients of ulcerative colitis suffer from this dreaded complication. The risk increases in patients who have had a long standing disease (> 8 years) and the lining of the colon is severely damaged. It is recommended that patients who have been suffering from ulcerative colitis involving the whole colon for more than 8 years, or patients in whom the ulcerative colitis has been restricted to only the left side of the colon for 12 to 15 years, should undergo a colonoscopy annually to see if there are any precancerous cells. This would help in early diagnosis of cancer paving way for early treatment. Apart from colon cancer, patients of ulcerative colitis run the risk of suffering from osteoporosis, arthritis, renal calculi, etc.

Medications for ulcerative colitis
The role of medications in ulcerative colitis is to control the symptoms and to achieve a remission. This helps in improving the quality of life of the patient. Some of the commonly used medications in this condition include: • Aminosalicylates: They form the first line of treatment for ulcerative colitis. Their main role is to control the inflammation. They are given in the form of oral pills, rectal suppositories or rectal enema depending upon the part of the gut that is involved. • Corticosteroids: They are used to control the inflammation in patients who not show adequate response to aminosalicylates. Steroids are administered as pills, through the intravenous route, as rectal suppositories, enema or foam according to the part of the gastrointestinal tract involved. The use of corticosteroids for long term is generally avoided because of the multiple side effects they produce like gain in weight, mood swings, high blood pressure, bone loss, increases chances of contacting infections, etc. • Immunomodulators: These medicines work by suppressing the immune system. They take 3 to 6 months to start acting and are reserved for patients not responding to aminosalicylates. They are given only to patients with severe form of ulcerative colitis as...
The role of medications in ulcerative colitis is to control the symptoms and to achieve a remission. This helps in improving the quality of life of the patient. Some of the commonly used medications in this condition include: • Aminosalicylates: They form the first line of treatment for ulcerative colitis. Their main role is to control the inflammation. They are given in the form of oral pills, rectal suppositories or rectal enema depending upon the part of the gut that is involved. • Corticosteroids: They are used to control the inflammation in patients who not show adequate response to aminosalicylates. Steroids are administered as pills, through the intravenous route, as rectal suppositories, enema or foam according to the part of the gastrointestinal tract involved. The use of corticosteroids for long term is generally avoided because of the multiple side effects they produce like gain in weight, mood swings, high blood pressure, bone loss, increases chances of contacting infections, etc. • Immunomodulators: These medicines work by suppressing the immune system. They take 3 to 6 months to start acting and are reserved for patients not responding to aminosalicylates. They are given only to patients with severe form of ulcerative colitis as they can cause multiple side effects.
- Important notification about information and brand names used in this slideshow!
- Photo courtesy of e-Magine Art by Flickr : www.flickr.com/photos/emagineart/4655344761/

Living with ulcerative colitis
A patient of ulcerative colitis can make certain modifications in his lifestyle in order to prevent flares. These include: • Dietary modifications: Avoiding dairy products, fatty foods and too much fiber in the diet can help in preventing flaring up of the symptoms. • Taking supplements: As absorption of vital nutrients from the gut is impaired in ulcerative colitis, it becomes necessary to include dietary supplements in order to prevent the deficiency of these nutrients. Some of these supplements include iron, folic acid, and calcium. • Including probiotics in diet: As the normal bacteria residing in the gut are destroyed in ulcerative colitis leading to frequent episodes of diarrhea, including probiotics in diet can help in replenishing the gut flora. Probiotics can be taken in yogurts, milk, soy beverages, etc. • Staying hydrated: As frequent diarrhea can lead to dehydration, it is imperative for the patients to drink adequate amount of water and staying well hydrated. • Apart from these factors, it is advisable for the patient to avoid stressful situations and give up smoking as both these factors can trigger an episode of ulcerative colitis.
- Important notification about information and brand names used in this slideshow!
- Photo courtesy of Bert Kimura by Flickr : www.flickr.com/photos/treevillage/3297205866/

Treatment options for patients with ulcerative colitis
Apart from medications and surgery, there are various other treatment options for patients suffering from ulcerative colitis. These include: • Biologic therapies: Also called as anti-tumor necrosis factor agents (anti-TNF agents), these are therapies reserved for people who not respond to conventional therapies. They act against tumor necrosis factors, proteins which induce inflammation. • Whipworm therapy: A recent study published in the journal Gastroenterology has found that 43% of patients suffering from ulcerative colitis improved when they ingested pig whipworm eggs for 12 weeks. • Surgical therapy: 25% to 40% patients of ulcerative colitis require surgical intervention despite being on regular medications. Some of these indications include toxic megacolon, uncontrolled bleeding from an ulcer, a fulminant attack of ulcerative colitis which is refractory to medication, or a sudden tear in the colon which requires urgent repair.
- Important notification about information and brand names used in this slideshow!
- Photo courtesy of Mercy Health by Flickr : www.flickr.com/photos/mercyhealth/6996690484/
























Your thoughts on this
Loading...