I'm an alcoholic, though my drinking hadn't been too heavy until September last year, when it escalated.
However, I have been experiencing certain "symptoms" that have been concerning me.
I'm due to have a liver function test done, but I was wondering if someone just tell me what the early symptoms may be of potential liver damage (not necessarily liver disease)?
I'm a medical student, so please explain it in medical and scientific terms.
Thanks! :D
However, I have been experiencing certain "symptoms" that have been concerning me.
I'm due to have a liver function test done, but I was wondering if someone just tell me what the early symptoms may be of potential liver damage (not necessarily liver disease)?
I'm a medical student, so please explain it in medical and scientific terms.
Thanks! :D
Loading...
OK then. Here it is.
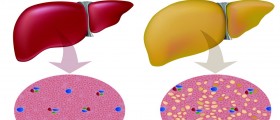
Alcohol causes a spectrum of liver injury that can progress from fatty liver to alcoholic hepatitis (often considered an intermediate stage) to cirrhosis.
Fatty liver, alcoholic hepatitis, and cirrhosis often are considered separate, progressive manifestations of alcoholic liver disease. Their features, however, often overlap.
Fatty liver (steatosis) is the initial and most common consequence of excessive alcohol ingestion. It is potentially reversible. Fatty liver is the accumulation of macrovesicular fat as large droplets of triglyceride that displaces the hepatocyte nucleus. Less often, fat appears in a microvesicular form as small droplets that do not displace the nucleus. Microvesicular fat represents mitochondrial damage. The liver enlarges, and the cut surface is yellow.
Alcoholic hepatitis (steatohepatitis) is a combination of fatty liver, diffuse liver inflammation, and liver necrosis (often focal), all in various degrees of severity. Cirrhosis may be present as well. The damaged hepatocytes either are swollen with a granular cytoplasm (balloon degeneration) or contain fibrillar protein in the cytoplasm (Mallory or alcoholic hyaline bodies). Severely damaged hepatocytes become necrotic. Collagen accumulation and fibrosis of the terminal hepatic venules compromise hepatic perfusion and contribute to portal hypertension. Histologic features that predict progression to cirrhosis include perivenular fibrosis, microvesicular fat, and giant mitochondria.
Cirrhosis is advanced liver disease characterized by extensive fibrosis that disrupts the normal liver architecture. The amount of fat present varies. Alcoholic hepatitis may coexist. The feeble compensatory attempt at hepatic regeneration produces relatively small nodules (micronodular cirrhosis), shrinking the liver. In time, particularly with abstinence, this can progress to macronodular cirrhosis.
Symptoms match the stage and severity of disease. Symptoms generally become apparent in patients during their 30s; severe problems appear about a decade later.
Fatty liver usually causes no symptoms. In 1⁄3 of patients, the liver is enlarged, smooth, and occasionally tender.
Alcoholic hepatitis ranges from a mild, reversible illness to a life-threatening disease. In moderate cases, patients usually are malnourished and present with fatigue, fever, jaundice, right upper quadrant pain, tender hepatomegaly, and, sometimes, a hepatic bruit. Their condition often deteriorates in the first few weeks of hospitalization. Severe cases may involve jaundice, ascites, hypoglycemia, electrolyte abnormalities, hepatic insufficiency with coagulopathy or portal-systemic encephalopathy, or other manifestations of cirrhosis. If severe hyperbilirubinemia > 20 mg/dL (> 360 μmol/L), prolonged PT or INR (unresponsive to vitamin K sc), and encephalopathy are present, the risk of death is 20 to 50%, and the risk of cirrhosis is 50%.
Cirrhosis may cause symptoms ranging from minimal to those of alcoholic hepatitis or the complications of end-stage liver disease. Commonly, portal hypertension (often with esophageal varices and upper GI bleeding, ascites, portal-systemic encephalopathy), hepatorenal syndrome, or even hepatocellular carcinoma is present.
In any chronic alcoholic liver disease, Dupuytren's contracture of the palmar fascia, vascular spiders, peripheral neuropathy, Wernicke's encephalopathy, Korsakoff's psychosis, and, in men, signs of hypogonadism and feminization (eg, smooth skin, lack of male-pattern baldness, gynecomastia, testicular atrophy) may be present. These manifestations more likely reflect the effect of alcoholism than of liver disease. Malnutrition may lead to enlarged parotid glands. Hepatitis C virus infection occurs in about 25% of alcoholics, a combination that markedly worsens the progression of liver disease.
Alcohol causes a spectrum of liver injury that can progress from fatty liver to alcoholic hepatitis (often considered an intermediate stage) to cirrhosis.
Fatty liver, alcoholic hepatitis, and cirrhosis often are considered separate, progressive manifestations of alcoholic liver disease. Their features, however, often overlap.
Fatty liver (steatosis) is the initial and most common consequence of excessive alcohol ingestion. It is potentially reversible. Fatty liver is the accumulation of macrovesicular fat as large droplets of triglyceride that displaces the hepatocyte nucleus. Less often, fat appears in a microvesicular form as small droplets that do not displace the nucleus. Microvesicular fat represents mitochondrial damage. The liver enlarges, and the cut surface is yellow.
Alcoholic hepatitis (steatohepatitis) is a combination of fatty liver, diffuse liver inflammation, and liver necrosis (often focal), all in various degrees of severity. Cirrhosis may be present as well. The damaged hepatocytes either are swollen with a granular cytoplasm (balloon degeneration) or contain fibrillar protein in the cytoplasm (Mallory or alcoholic hyaline bodies). Severely damaged hepatocytes become necrotic. Collagen accumulation and fibrosis of the terminal hepatic venules compromise hepatic perfusion and contribute to portal hypertension. Histologic features that predict progression to cirrhosis include perivenular fibrosis, microvesicular fat, and giant mitochondria.
Cirrhosis is advanced liver disease characterized by extensive fibrosis that disrupts the normal liver architecture. The amount of fat present varies. Alcoholic hepatitis may coexist. The feeble compensatory attempt at hepatic regeneration produces relatively small nodules (micronodular cirrhosis), shrinking the liver. In time, particularly with abstinence, this can progress to macronodular cirrhosis.
Symptoms match the stage and severity of disease. Symptoms generally become apparent in patients during their 30s; severe problems appear about a decade later.
Fatty liver usually causes no symptoms. In 1⁄3 of patients, the liver is enlarged, smooth, and occasionally tender.
Alcoholic hepatitis ranges from a mild, reversible illness to a life-threatening disease. In moderate cases, patients usually are malnourished and present with fatigue, fever, jaundice, right upper quadrant pain, tender hepatomegaly, and, sometimes, a hepatic bruit. Their condition often deteriorates in the first few weeks of hospitalization. Severe cases may involve jaundice, ascites, hypoglycemia, electrolyte abnormalities, hepatic insufficiency with coagulopathy or portal-systemic encephalopathy, or other manifestations of cirrhosis. If severe hyperbilirubinemia > 20 mg/dL (> 360 μmol/L), prolonged PT or INR (unresponsive to vitamin K sc), and encephalopathy are present, the risk of death is 20 to 50%, and the risk of cirrhosis is 50%.
Cirrhosis may cause symptoms ranging from minimal to those of alcoholic hepatitis or the complications of end-stage liver disease. Commonly, portal hypertension (often with esophageal varices and upper GI bleeding, ascites, portal-systemic encephalopathy), hepatorenal syndrome, or even hepatocellular carcinoma is present.
In any chronic alcoholic liver disease, Dupuytren's contracture of the palmar fascia, vascular spiders, peripheral neuropathy, Wernicke's encephalopathy, Korsakoff's psychosis, and, in men, signs of hypogonadism and feminization (eg, smooth skin, lack of male-pattern baldness, gynecomastia, testicular atrophy) may be present. These manifestations more likely reflect the effect of alcoholism than of liver disease. Malnutrition may lead to enlarged parotid glands. Hepatitis C virus infection occurs in about 25% of alcoholics, a combination that markedly worsens the progression of liver disease.
Loading...