Table of Contents
Don't guess. Test!
That's the new motto of the "Don't Guess. Test." campaign started by the Bonnie J. Addario Lung Cancer Foundation (ALCF), in collaboration with Foundation Medicine and Friends of Cancer Research and 13 other American cancer research foundations to encourage the use of genetic testing in cancer treatment. Even though it's now possible to sequence all 20,000 genes in the human body, much of medical treatment for cancer remains a matter of guesswork.
No chemotherapy, immunotherapy, or radiation treatment works in every case. (Neither is there any natural treatment that is a cure for all cancers, although some natural treatments work better than chemo for some people who have certain kinds of cancers.) For decades, oncologists have relied on subtle cues from their patients and years of experience in the clinic to choose the best therapies for their patients, usually with less than a 50 percent success rate, often relying on multiple drugs with multiple side effects. Genetic testing may enable a more precise, more successful, more easily tolerated regime of cancer treatment by answering questions such as these:
- Does the cancer patient have specific genes that predict the success or failure of a specific drug?
- Are there mutations in the cancerous tumor that indicate that a typically line of treatment won't work but maybe an off-label drug will?
- Does whole genome sequencing or genome mapping (identifying all of a person's genes) as a whole offer insights into the best holistic treatment for a patient?
Most cancer patients in the United States, who, despite the country's deficiencies in other areas of medicine, have a greater chance of survival than cancer patients in other countries, still get a kind of piecemeal testing to help their doctors choose the right cancer drugs. Cancerous tumors generate proteins that can serve as biomarkers, substances that can be analyzed with blood tests.
The problem with using biomarkers is that they aren't particularly precise tools of diagnosis. Here are some examples:
- Alpha Fetoprotein (AFP) is a protein made by the fetus that disappears after birth. It also appears in 60 percent of men in the early stages of testicular cancer, which is to say, it fails to appear in 40 percent of men in the early stages of testicular cancer. It can also be produced by the body if there is hepatitis.
- Cancer Antigen 125 (CA-125) is a protein that appears in 50 percent of women in the early stages of ovarian cancer. It also fails to appear during the early stages of 50 percent of women who have ovarian cancer. It can be made by healthy cells.
- Cancer Antigen 15-3 (CA-15-3) appears in 95 percent of women who have advanced breast cancer, but in only in 19 percent of women who have early-stage breast cancer. It is also produced in liver disease, tuberculosis, and sarcoidosis.
- Cancer Antigen 19-9 (CA 19-9) appears in 60 to 70 percent of all cases of biliary cancer and 90 percent of cases of pancreatic cancer. However, it can also appear when the problem is non-cancerous pancreatitis or some non-cancerous liver disease.
READ Night shifts increase your ovarian cancer risk
- Prostate-specific antigen (PSA) is elevated in 70 percent of cases of prostate cancer, but it isn't in 30 percent of cases. Because PSA is actually a measure of inflammation, levels can go up to "cancerous" levels just because the doctor did a prostate exam before blood was drawn.
- Gupta, S. Insurers wrestle with cost, efficacy of genetic testing. MedPage Today, 3 February 2016.
- Hackethal, V. Genomic Sequencing Shows Benefit for Children With Cancer. Medscape Oncology. 3 September 2015.
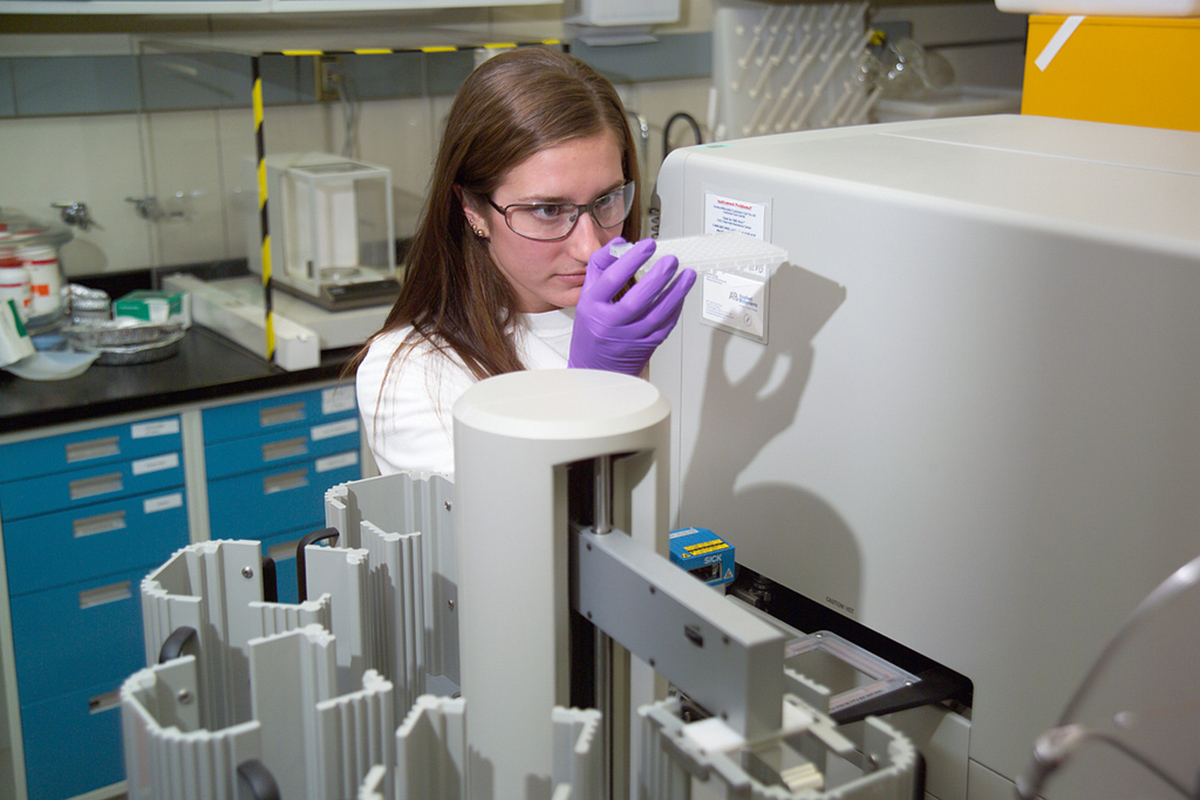
- Photo courtesy of inl: www.flickr.com/photos/inl/3637156598/
- Photo courtesy of beigephotos: www.flickr.com/photos/beigephotos/2299600717/
- Photo courtesy of inl: www.flickr.com/photos/inl/3637156598/


Your thoughts on this