An open discectomy is the most common surgical treatment for ruptured or herniated discs of the lumbar spine. This surgery is used to remove a part of the damaged disc which is relieving the pressure on the nerve tissue and alleviating the pain.
The surgery involves:
- A small incision in the skin over the spine
- The removal of some ligament and bone material
- The removal of some of the disc material.
Doctors have been performing open discectomy procedures for nearly 80 years. Modern medical technologies like magnetic resonance imaging (MRI) and computerized tomography (CT) have allowed medical professionals to refine the procedure further.
This operation has an excellent success rate of 80 to 90 percent. Studies have also shown that discectomy operations are more successful in people with radicular pain than in those with low back pain.
Pathophysiology of the condition
Vertebral discs are cushioning and connecting materials that lie between the bones of the spine. When the outer wall of this disc becomes weakened through age or injury, it may tear and eventually bulge out. This is called disc herniation, disc prolapse, or a slipped or bulging disc.
Once the inner disc extends out it can press sensitive nerve tissue in the spine. This then causes weakness, tingling, or pain in the back area and into one or both legs. Herniated disks can affect your ability to perform everyday tasks and can cause severe pain. Although the pain is simply unbearable at times, herniated disks aren't likely to result in paralysis.
Proper indications for a discectomy
Not all patients with herniated discs are candidates for the open discectomy procedure. This operation is usually the option of last resort if other possible treatments such as rest, physical therapy, anti-inflammatory medications, and epidural injections didn’t offer relief or improve functionality.
Before the operation, the doctor may order diagnostic tests, such as X-rays, MRI or a CT scan, to verify the source of the pain. If a diagnosis of a herniated disc is confirmed, an open discectomy may be recommended.
Open disectomy: How is it done?
This operation is performed under general anesthesia.
The surgeon makes a one-inch incision in the skin over the affected area and removes the muscle tissue above the bone.
In some cases, bone and ligaments may also need to be removed for the surgeon to be able to visualize the bulging disc without damaging the nerve tissue. This is called a laminectomy.
During a laminotomy a portion of lamina is removed to relieve pressure on a nerve or allow the surgeon access to a disk that's pressing on a nerve. When the surgeon finishes all the preoperative preparations, the section of the disc that is protruding from the disc wall will be removed. This should relieve all the symptoms and allow the patient to enjoy a higher quality of life. No implants and no artificial material is used to replace the disc tissue that is removed.
Microdiscectomy and arthroscopical approach
This operation can also now be performed arthroscopically. This means that the surgical team conducts the procedure through a smaller incision using specialized tools under local anesthesia. A microdiscectomy on the other hand is performed using a special microscope or magnifying instrument to view the disc and nerves. The magnified view makes it possible for the surgeon to remove herniated disc material through a smaller incision, thus causing less damage to surrounding tissue.
Micro-Endoscopic Discectomy (MED)
During this procedure, a machine called fluoroscope which projects live x-ray pictures onto a screen is brought into the operation room. The disc space is confirmed using the fluoroscope, and a long acting, local anesthetic is injected through the muscle and around the bone protecting the disc.
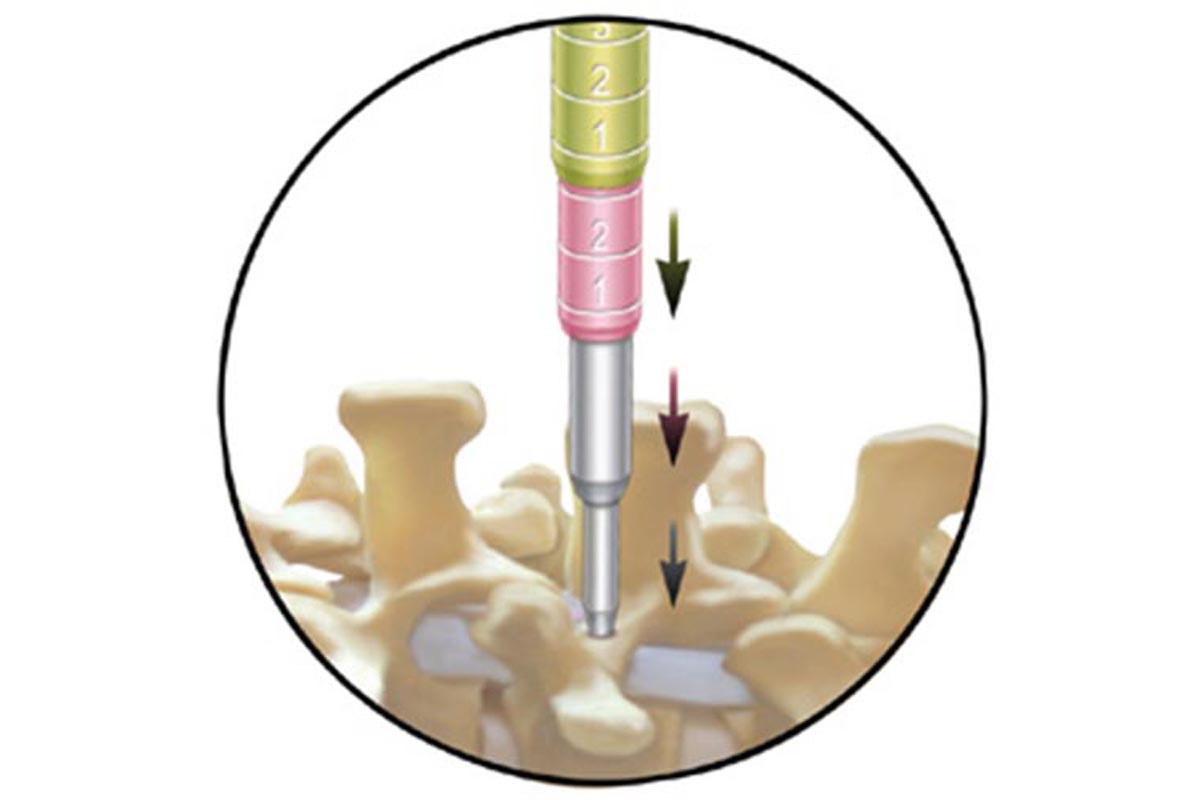
A surgeon then makes a small incision through which the thin wire is placed and lowered until it touches the bone. Progressively larger dilators are brought down on top of one another following the wire. By the time the 4th or 5th dilator is placed, the muscles are stretched to an opening roughly the size of a nickel.
The retractor is held in place by a mechanical arm attached to the table. Finally, the endoscope with a camera is attached to the edge of the working channel. This projects an image onto a TV screen to allow the surgeon to see what is happening. This allows for microscopic manipulation and removal of the tissues which could be extremely helpful.
Discectomy with bone-grafting
A cervical discectomy is the most common surgical procedure to treat damaged cervical discs. When the damaged disc is localized in the neck, the operation is called anterior because the cervical spine is reached through a small incision in the front of the neck.
During the surgery, the soft tissues of the neck are separated and the disc is removed. In order to maintain the normal height of the disc space, the surgeon may choose to fill the space with a bone graft. A bone graft is a small piece of bone, which can either be taken from the patient's body or from a donor or bone bank. This bone fills the disc space and ideally will join or fuse the vertebrae together.
What happens after a discectomy surgery?
After a discectomy, a patient may feel pain at the site of the incision. Patients should be aware that the original pain may not be completely relieved immediately after the surgery; it takes time to discover whether the surgery was successful. In most cases, patients are prescribed analgesics to offer pain relief during the postoperative period.
Once the patient is discharged from the hospital, the physician in charge may prescribe physical therapy. No patient should attempt to drive an automobile until it is approved by a physician.
Walking is the first physical activity a patient should attempt after undergoing a discectomy procedure. In a few weeks, he or she may be allowed to ride a bike or swim. Formal physical therapy may speed up your recovery and make it more complete.
Possible complication of discectomy
Possible complications from open discectomy include:
- bleeding
- infection
- spinal fluid leak
- injury to the veins and arteries near the spine
- injury to the nerve tissue of the spine or its surrounding protective layer
- recurrent disc herniation which occur in approximately 5% to 10% of open discectomy cases
Prognosis
Most people with jobs that are not physically challenging can return to work in two to four weeks or less. Those with jobs that require heavy lifting or operating heavy machinery may need to wait at least six to eight weeks after surgery to return to work. Again, physical therapy may have an important role in your recovery. Full recovery after a discectomy can be expected within eight to twelve weeks in most cases.
Discectomy - pros and cons
Disectomy Pros
- Open discectomy allows the surgeon the greatest ability to see and explore the surgical site
- It relieves all the symptoms in almost 90% of the cases
- Only ultimate long-run solution of back pain
- Discectomy provides faster pain relief than non-surgical treatment
- X-ray exposure is minimal
- Recovery from a discectomy is fairly quick in most patients
- Pain following surgery is usually well controlled with oral pain medication
Disectomy Cons
- Pain at the site of the incision
- Possible complications such as bleeding, infection, spinal fluid leak, injury to the veins and arteries near the spine
- Recurrent disc herniation
- Fever, weakness or numbing of the legs, or problems urinating
- www.spine.org
- en.wikipedia.org/wiki/Anterior_cervical_discectomy_and_fusion
- www.spineuniverse.com
- image: www.texasspinecenter.com

