Once a prosperous if somewhat complicated country, the break-up of Yugoslavia — meaning "nation of Southern Slavs", and located on the Balkan peninsula east of Italy — swept the six new countries that emerged into rough waters. Bosnia and Herzegovina, Serbia and Croatia, in particular, experienced first-hand how messy the disintegration of a society of peoples that should perhaps never have become one nation can be, in the form of a brutal civil war that reignited generations-old ethnic tensions, and economic despair.

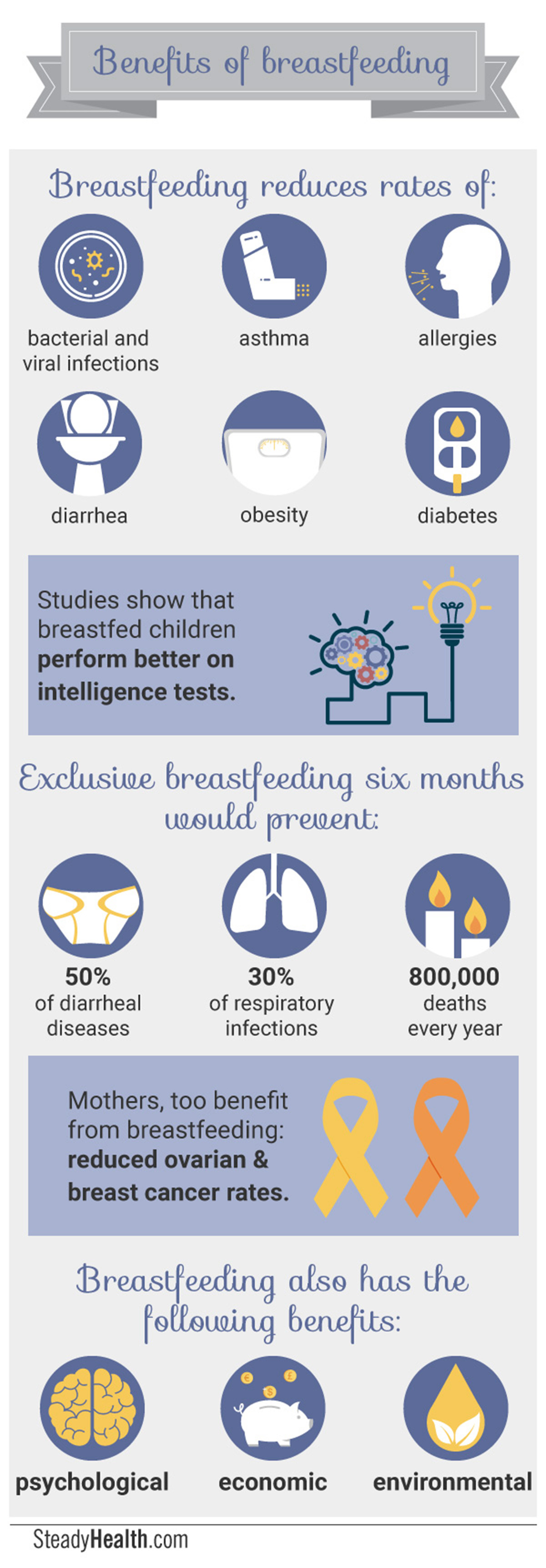
Two and a half decades on, these three countries are looking to the future, and there's arguably little that's more future-oriented than having babies. Breastfeeding, research shows time and time again, is more than a mode of infant feeding — it offers life-long health benefits to both babies and their mothers.
SteadyHealth investigated the personal attitudes mothers, their social circles, and their healthcare providers have towards breastfeeding in Serbia, Croatia, and Bosnia and Herzegovina. These countries are all part of the World Health Organizations' European region, the WHO region with the lowest global breastfeeding rates. In the case of Bosnia and Herzegovina, we surveyed the Croat-Bosniak Federation of Bosnia and the predominantly Serbian region of Republika Srpska separately to gain insights into potential differences in attitudes towards breastfeeding within these two administrative entities. The surveys were conducted in October 2016.
READ Got Breast Milk? A Third Of Serbian Mothers Say They Don't, SteadyHealth Survey Finds
Understanding why more mothers don’t breastfeed for longer is the key to improving breastfeeding rates. Pre-existing national data offers insights into breastfeeding rates in this region, but fails to reveal the underlying reasons for which mothers cease breastfeeding prematurely.
READ Nursing The Future: Croatia Regional Breastfeeding Success Story, SteadyHealth Survey Finds
The four surveys focused on large urban centers and the more rural areas directly surrounding them, allowing us to encompass a great variety of socio-economic groups. Serbia and Bosnia and Herzegovina are both classified as Upper Middle Income countries, with Croatia being considered a High Income country, according to the World Bank classification system. Our research was entirely self-funded without any conflicts of interest to declare — our goal as simple as delving deeper into the reasons for which mothers give up on breastfeeding.
Breastfeeding Practices Within Serbia, Bosnia, And Croatia
Across all four regions, an overwhelming majority of respondents reported initiating breastfeeding: 92.26% in Serbia, 95.8% in the Federation of Bosnia and Herzegovina (in the rest of the text, FBiH), 91.67% in the Republic of Srpska entity of Bosnia and Herzegovina (in the rest of the text, Srpska), and 95.74% in Croatia.
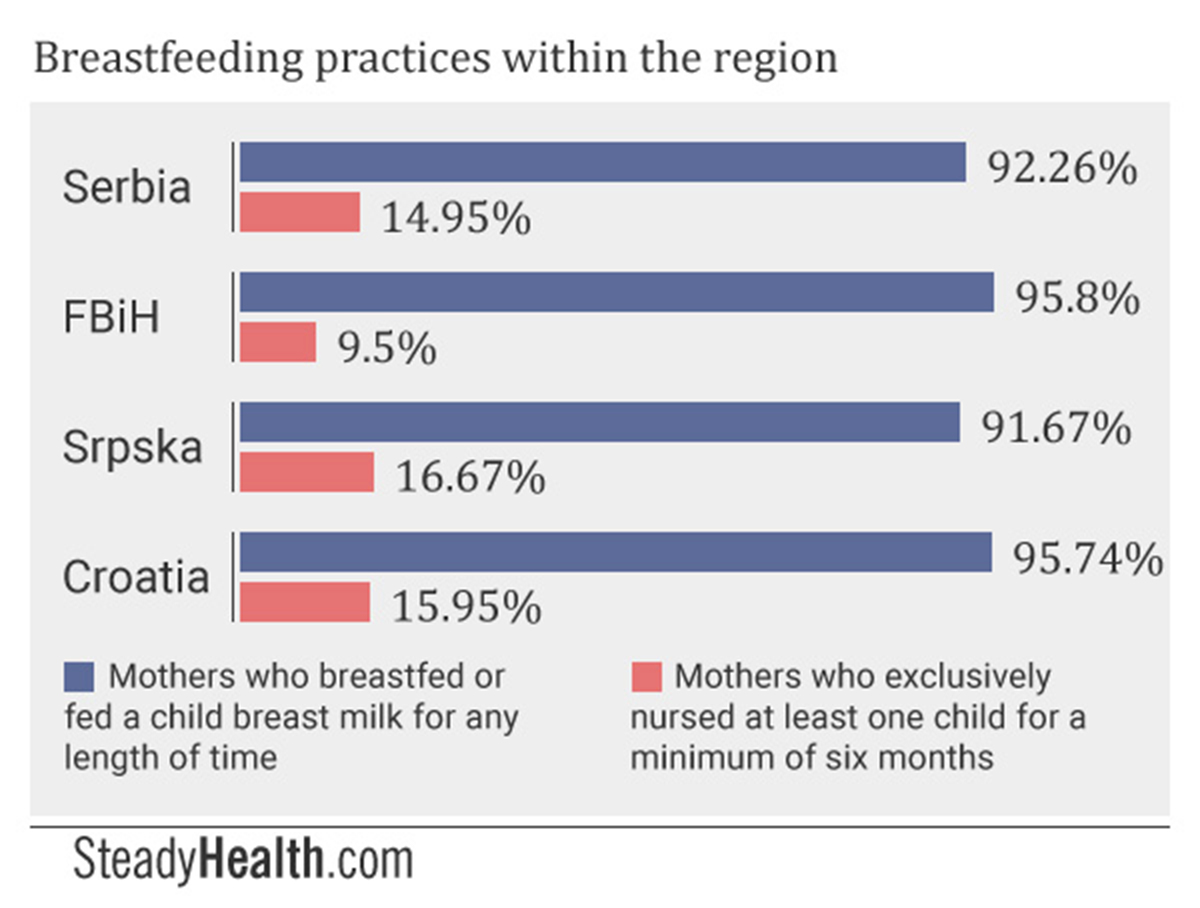
The World Health Organization strongly recommends that infants be breastfed or fed breast milk exclusively during the first six months of their lives, meaning no formula, no supplementation with water — simply said, nothing but breast milk. Among respondents in Serbia, 14.95% reported that they exclusively nursed at least one child for a minimum of six months, slightly more than the 13.7% suggested by national data from 2010. National data from the whole of Bosnia and Herzegovina showed that 17.6% of mothers exclusively breastfeed their children up to six months of age, while 9.5% of our survey respondents based in the Federation of BiH and 16.67% of Srpska-based respondents did. Almost 16% of Croatian participants said that they followed the WHO’s guidelines on breastfeeding with at least one child, though national data from 2011 showed that 54.2% of mothers did.
When mothers who self-identified as not having breastfed answered our question delving more deeply into the reasons why, those who nursed their babies for a very short amount of time responded alongside those who never breastfed at all.
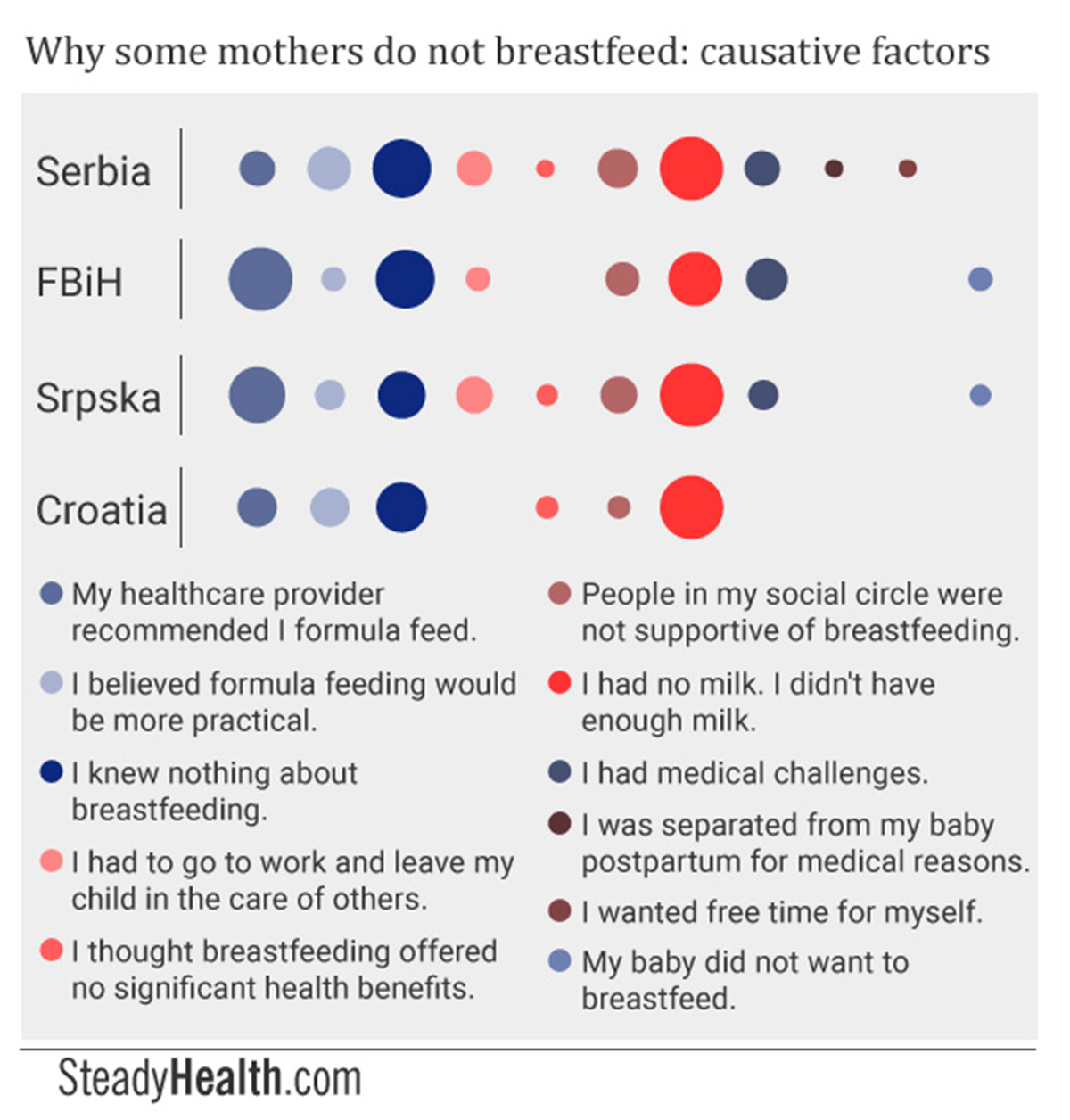
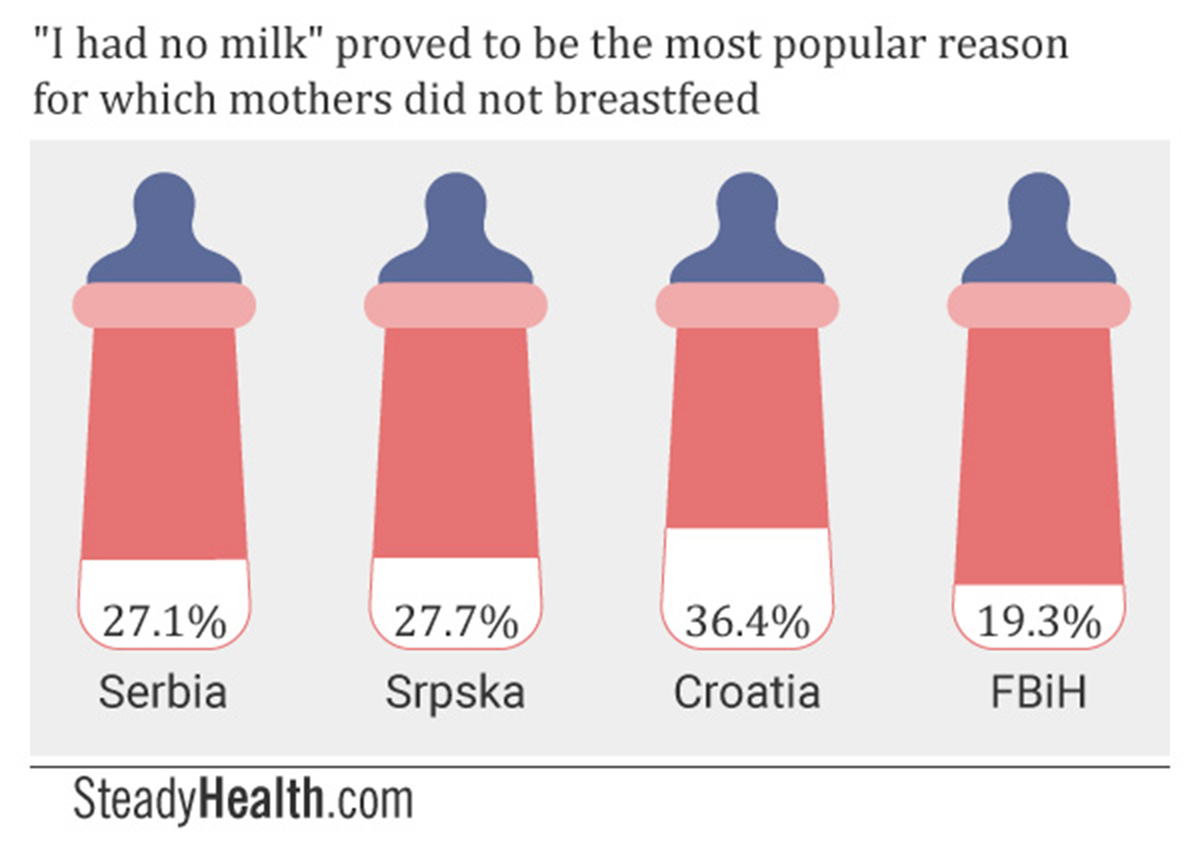
Participants were offered a multiple-choice answer format and in addition received the chance to tell us why they did not breastfeed in their own words. In three of the four surveyed regions, “I didn’t have breast milk” or “I had an insufficient amount of breast milk to feed my baby”, an answer that was not part of our multiple choice list, proved to be the most popular reason for formula feeding. That is, 27.1% of Serbian respondents, 27.27% of Srpska respondents, and 36.36% of Croatian mothers who took part in our survey responded this way. Only in FBiH was “my healthcare provider recommend I formula feed” the most prevalent reason for not breastfeeding.
This could partially be explained by our findings that significant numbers of mothers were unable to breastfeed on demand while in hospital because their babies were in the hospital nursery, and that healthcare providers frequently formula feed babies without their mothers’ consent.
What else could be behind these beliefs, though? SteadyHealth spoke to Milena Popevic, a peer-to-peer breastfeeding advisor with the popular “Association of Parents”, from Serbia. Popevic explained:
"I believe it is because maternity hospital staff ‘fills their heads’ with this notion. It’s not unusual for staff to say: ‘You got nothing; you won’t be able to breastfeed’. Or they say, ‘we have to use formula because your milk hasn't come in yet’, though they already have colostrum.
These women go home with the idea that they don’t have enough milk. If their babies also don’t latch on properly, it is possible that they aren’t taking in enough milk, and that they become nervous and cue that they want to nurse all the time. Mothers then conclude that their babies are hungry and that they don’t have milk because their babies keep wanting to nurse."
“Stereotypical” reasons for which mothers choose formula over breast milk, such as believing formula to be more practical, wanting free time for oneself, and having to go to work and leave the baby in the care of others, appeared surprisingly low down on the list of reasons for which participants did not breastfeed.
Across all four regions, significant numbers of mothers did give "I knew nothing about breastfeeding" as the reason for which they chose formula: 22.9% in Serbia, 23% in FBiH, 15.15% in Srpska, and 22.73% in Croatia.
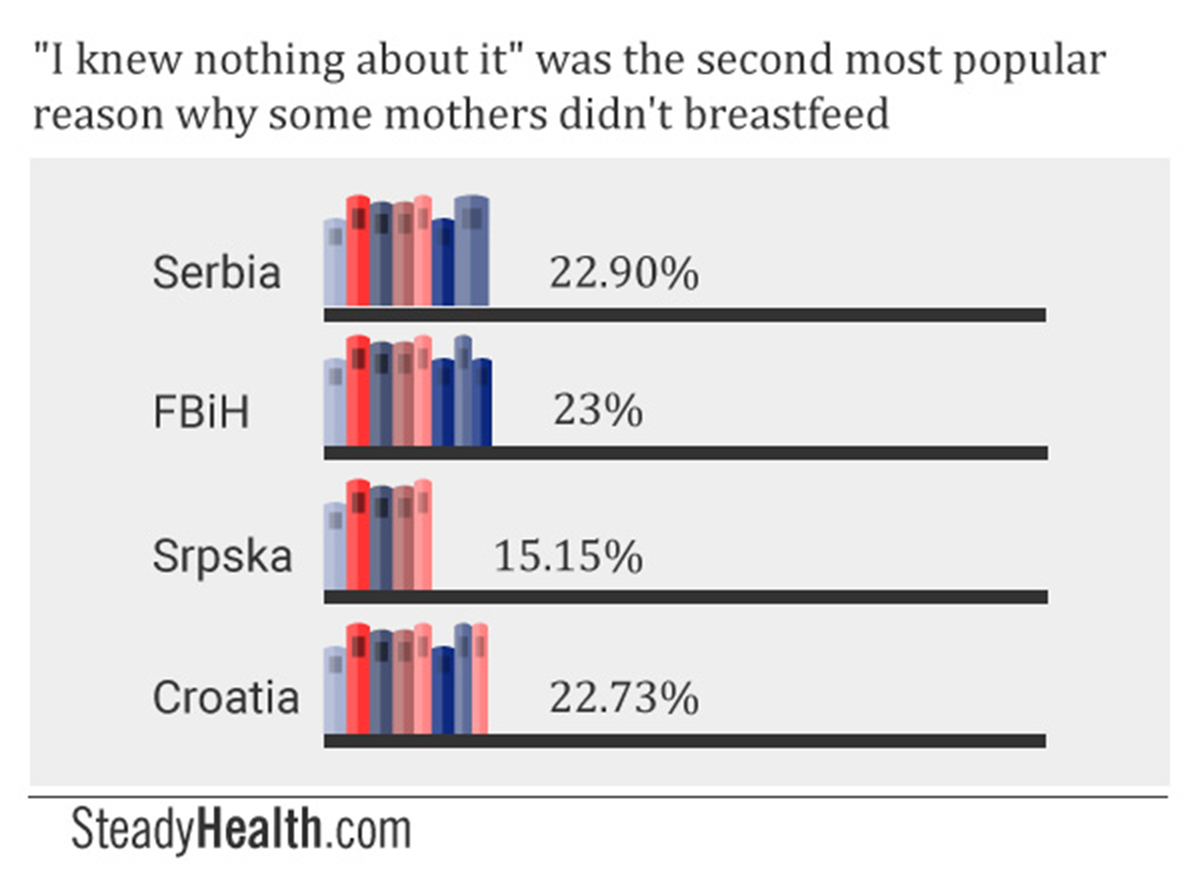
Across all four regions, significant numbers of mothers did give “I knew nothing about breastfeeding” as the reason for which they chose formula: 22.9% in Serbia, 23% in FBiH, 15.15% in Srpska, and 22.73% in Croatia.
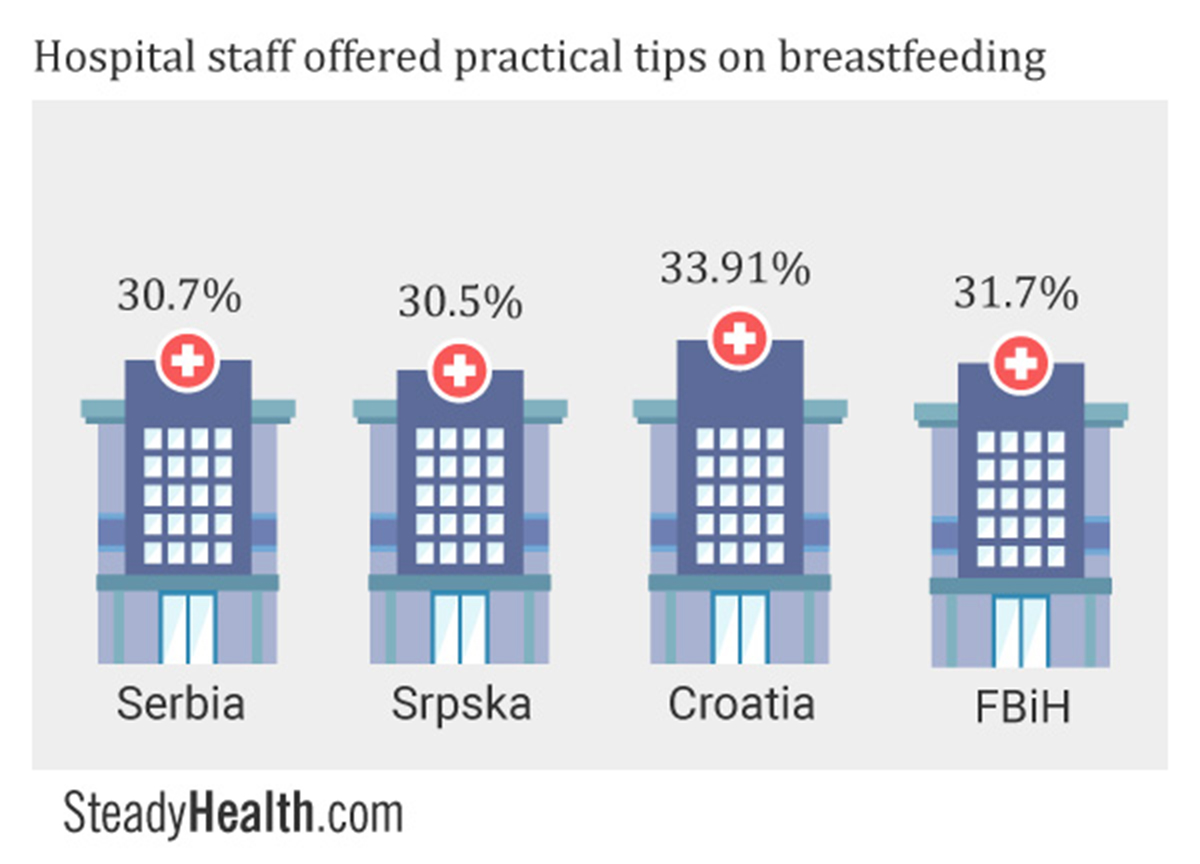
Among the group of women who self-identified as having breastfed, around a third of women reported that they received practical tips on succeeding at nursing within the maternity hospital. Likewise, 30.42%, 23%, 21.99%, and 28.16% of women in these same territories shared that they had encountered breastfeeding challenges of any kind but received healthcare provider help to overcome them.
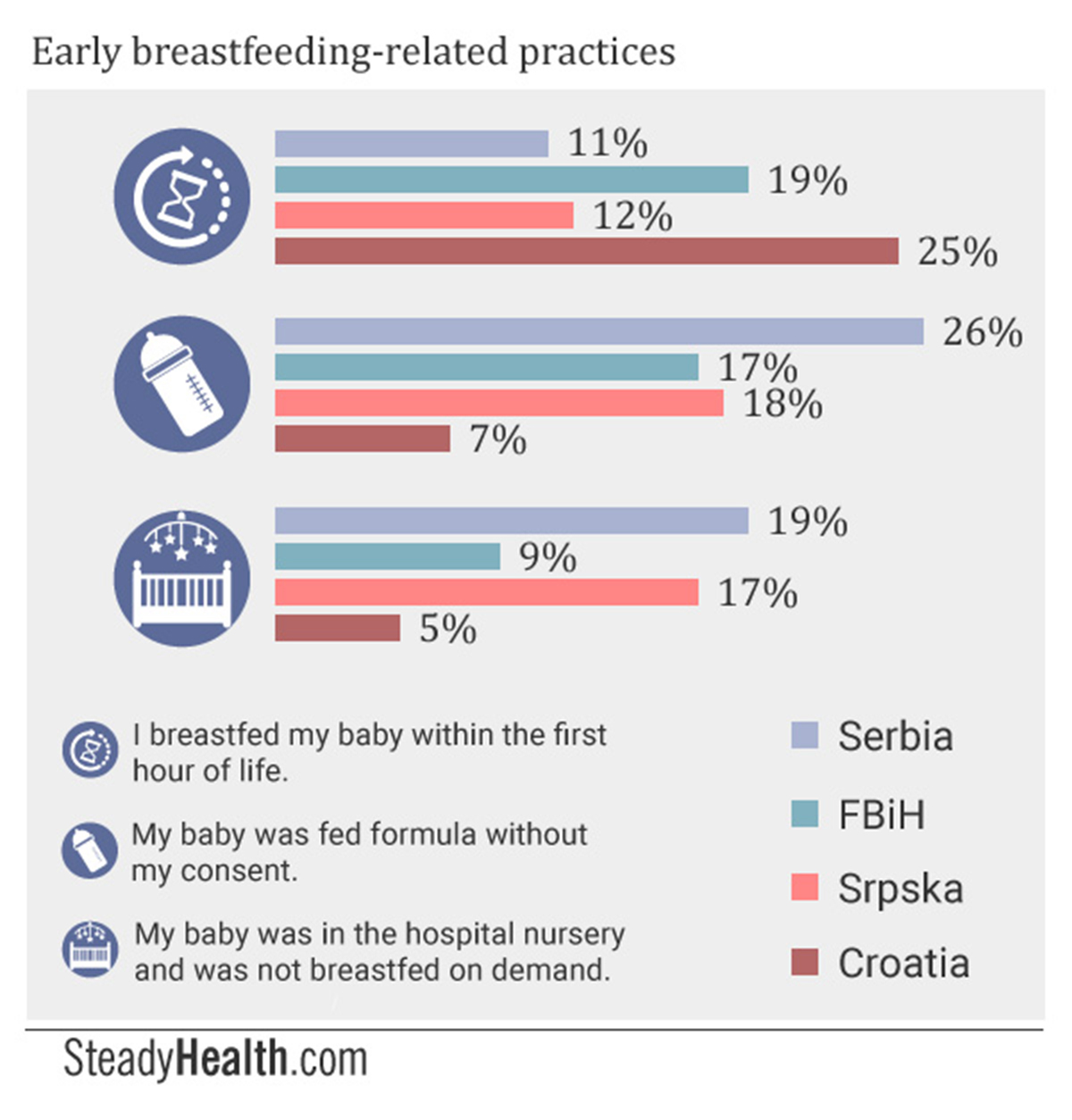
In FBiH, however, a lower 18.9% of respondents were given the chance to nurse their babies within the first hour, while 12.06% were able to do this in Srpska. Serbia had the lowest rate of breastfeeding initiation within at hour, 7.69%
Within Serbia, 17.48% of participants’ babies were fed formula without their consent by healthcare staff, while 18.7% were unable to feed their babies on demand as they were placed in the hospital nursery. The same held true for 30.5% and 17.02% respectively in Srpska. In FBiH, 31.7% of participating mothers also responded that their baby was given formula without their permission, though only 8.8% said they were not able to feed their babies as necessary because they were in the nursery. In Croatia, almost 34% of mothers shared that their babies were given formula without their consent, but again, a much lower percentage, 4.6%, missed out on the chance to nurse their babies on demand due to being separated from them.
We asked Ivana Dimitrijevic-Robertson, a La Leche League International leader from Serbia, to elaborate on this situation. She shared:
"I don't believe there are many obvious formula promotion code breaches in Serbian hospitals today, though I believe there must be backroom deals with individual pediatricians and pediatric nurses taking place. It is very common, for example, that mothers of newborns experience some pressure from the health visitors who visit the mothers at home within the few days following hospital release to offer a particular brand of formula to the baby without indicating a clear reason, or assessing the breastfeeding dyad appropriately.
It is hard to understand the real motivation behind this. It could be a lack of training, but I suspect subtle corruption to be the real reason behind most cases. I don't believe many maternity care providers genuinely believe formula to be a better way of feeding infants, but I think suspicion in the mother's ability to breastfeed is much more common than support. A 'fed is best' sort of attitude is also very common, which seems to imply that a large number of women aren't able to meet their babies' nutritional needs by breastfeeding, and also that formula is of equal nutritional value, if not better than the mother's milk. Again there are many reasons for this sort of attitude, but it boils down to a systemic disregard for motherhood."
Perceived Breastfeeding-Related Healthcare Provider Competence
In order to find out how knowledgeable our participants believed their healthcare providers to be about breastfeeding, we presented them with an open-ended question.
Our results were as follows:
-
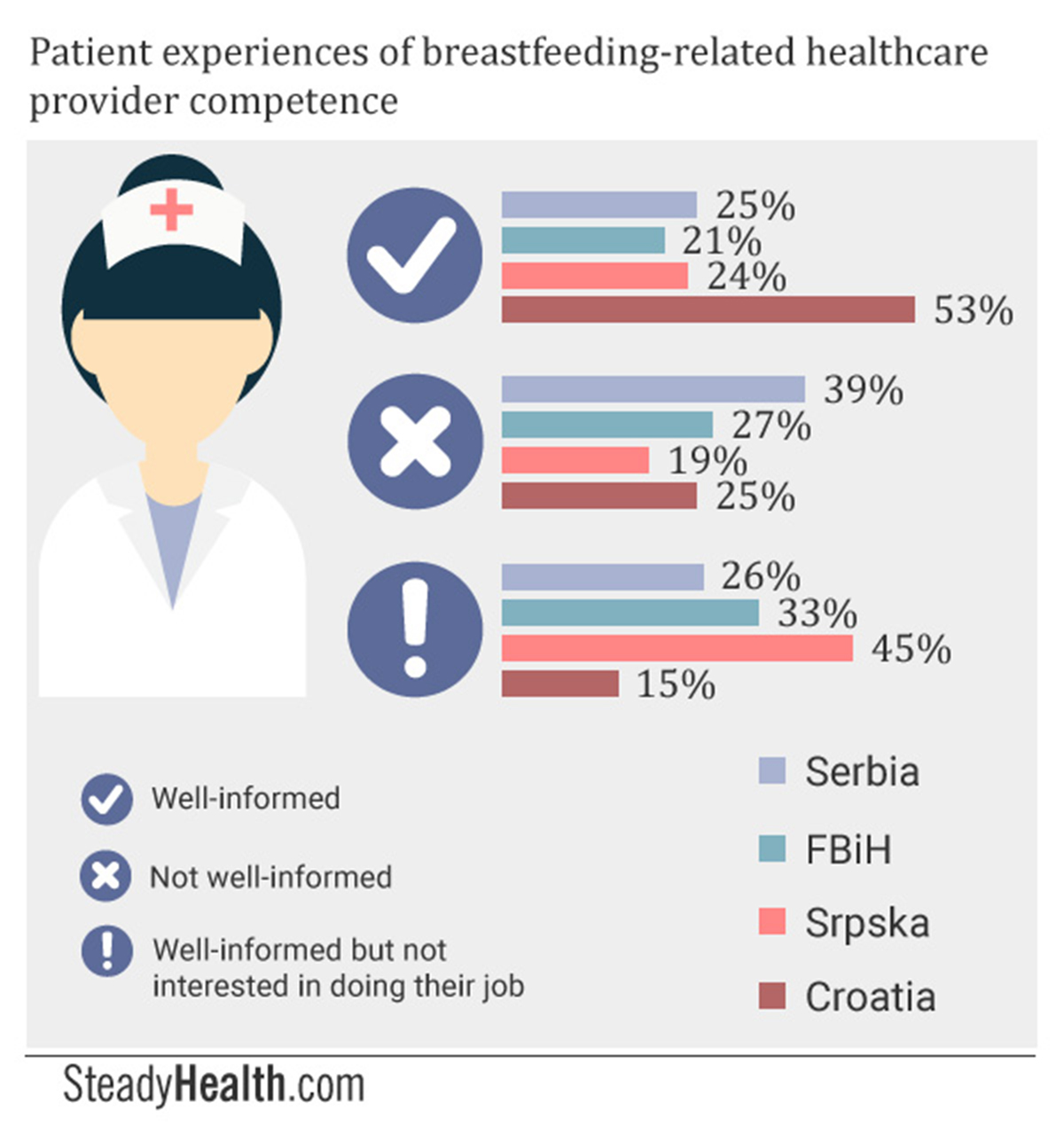
In Serbia, a quarter of participants said they believed their healthcare providers to be well-informed about the benefits of breastfeeding, about the possible complications mothers might encounter, and about ways in which these challenges could be overcome. A full 39% thought their healthcare providers ill-informed.
-
In the Federation of BiH, 20.7% believed their healthcare providers to be well-informed, while 27.3% held that they were not knowledgeable enough.
-
In Srpska, a higher percentage, 24.36%, thought that their healthcare providers were sufficiently knowledgeable about breastfeeding than not (19.12%).
-
Croatia was the only region in which a majority of participants, 52.94%, had confidence in the knowledge of their healthcare providers. A full quarter still believed that the staff involved in their maternity care did not know enough about breastfeeding to be able to adequately support them, though.
A total of 44.87% of participants from Srpska, 32.5% from FBiH, and 26% from Serbia, responded this way. Meanwhile, our Croatian respondents worded the same idea slightly differently, using phrases such as “they are not patient enough”, or “they do not take the time to show each mother how to breastfeed successfully”. In this case, a significantly lower 14.71% held this view.
We also asked our participants to share examples of the kind of breastfeeding-related care they received. We explicitly prompted respondents to talk about both positive and negative experiences. Whether because high-quality care tends to be taken for granted and negative experiences are simply more memorable, or because negative experiences indeed dominated among participants, the majority of mothers did not share positive experiences.
Some of their responses include:
-
“I was prescribed medication that was incompatible with breastfeeding.” (FBiH.)
-
"All healthcare providers I came into contact with are very much in favor of breastfeeding." (Serbia.)
-
“One midwife told me, soon after I gave birth, that I have neither breasts nor milk and that all I’ve got is water.” (Srpska.)
-
“A doctor asked me: ‘Would you like me to prescribe you medication to make your milk stop, if you don’t intend to nurse?’” (Croatia.)
-
"When I told a pediatrician that my 18 month old was still nursing, he told me I was creating a living Oedipus complex." (Serbia.)
-
“They’re not that interested. If you think you don’t have enough milk… there’s always formula, particularly the brand they will receive a commission from recommending.” (FBiH.)
-
“My health visitor told me that I had to drink milk to make milk.” (Croatia.)
-
"Nurses told me that breastfeeding small babies doesn't meet their needs and that they'd feed them formula right after." (Serbia.)
-
“I was told to breastfeed once every three hours, not on demand.” (Srpska.)
SteadyHealth asked Dr Gordana Mucibabic, a pediatrician at the private hospital Jelena in Banja Luka, Republika Srpska, what she thought of these findings. She answered:
"Despite the fact that we're talking more about the benefits of breastfeeding and the differences between breast milk and formula than ever before, it also seems to me that breastfeeding rates are at an all-time low in this region. Why is that? Like every other problem, this too is multifactorial: factors surrounding mothers, newborns and their social circles are involved, as well as the fact that any labor and delivery induces stress. The breasts themselves can be engorged and painful, and the nipples sensitive. Then there are social factors, in which people tell a new mother: 'Why are you suffering through this? Just give your baby a bottle, can't you see you don't have enough milk?'
I'll tell you that less than 1% of mothers who give birth at our hospital decide not to breastfeed for at least three months. How do we achieve this? Through workshops that explain the practical and theoretical side of breastfeeding during pregnancy, encouraging mothers to nurse right after their baby's birth depending on their health condition, and having a team at our disposal to ensure breastfeeding success in a comfortable environment during the first few days.
You asked why so many mothers believe they don' have milk, and why they think their healthcare providers are not devoted enough. I can't comment on the situation in clinics besides our own, but I believe the answers to the following questions would reveal all:
- Are expectant mothers well-informed? What percentage attends prenatal classes?
- How devoted are healthcare providers? If not very, why not? Are we talking about a lack of goodwill, ambitions, apathy, insufficient wages, an unrealistic workload, or something else?
- Are babies placed on the mother's chest right away?
- How much time do healthcare providers spend helping to get lactation started?
- How many times do health visitors see new mothers and how effective are those visits?
- Is our society able to offer adequate healthcare to new mothers and babies?
- Are mothers able to focus solely on nursing their babies or do they have existential worries, such as what they should do if their employer asks them to return to work early?
- How patient and helpful are new mothers' relatives?
- How educated are healthcare providers?
- Do pharmaceutical companies pressure healthcare workers to promote formula?"
Social Attitudes Mothers Serbia, Bosnia, And Croatia Encounter About Breastfeeding
What opinions and beliefs did our participants encounter within their social circles? We asked both those who breastfed for any length of time, and those who did not.
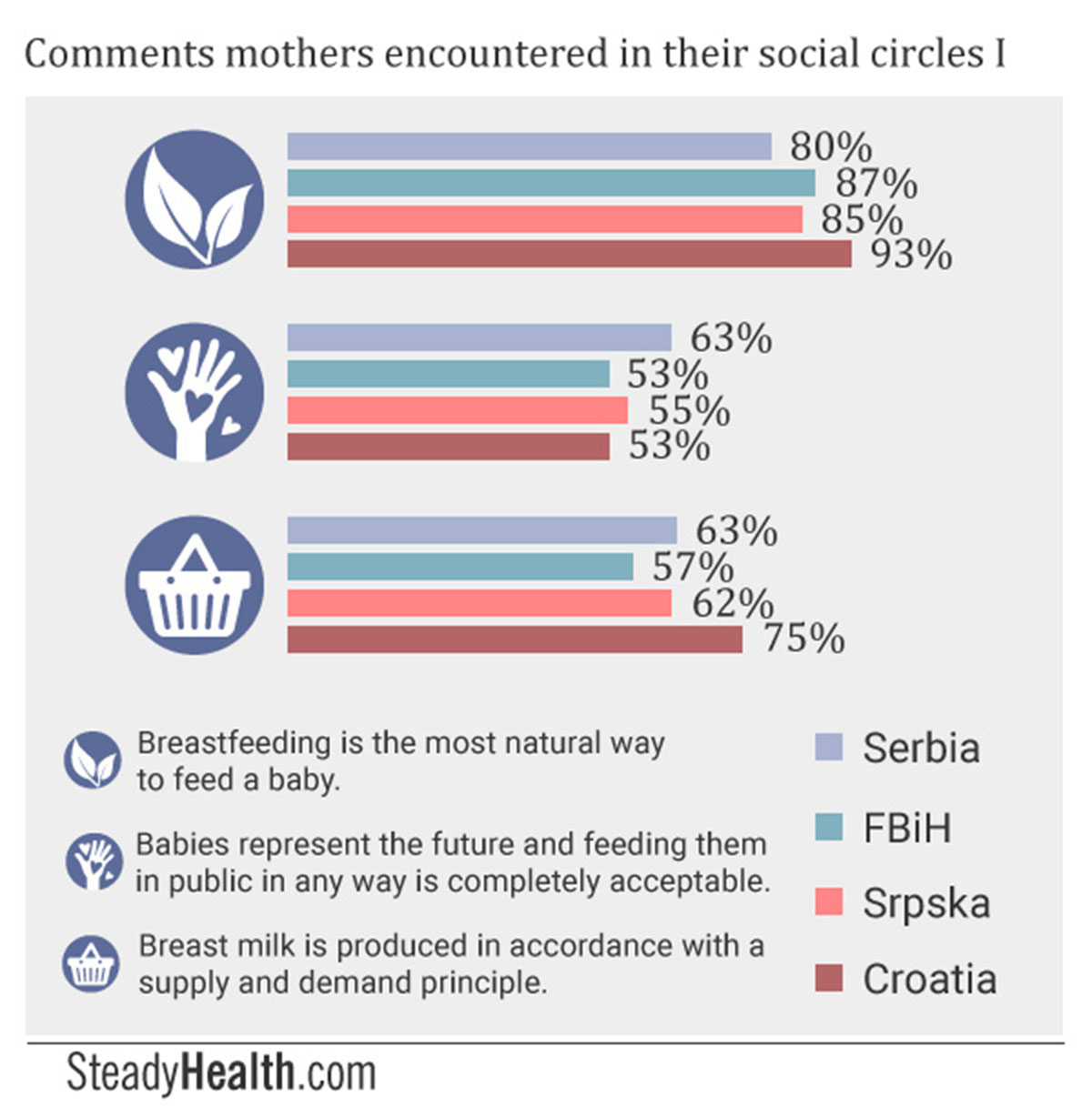
We found out that an overwhelming majority of mothers had heard the idea that breastfeeding was the most natural way to feed a baby from their friends and relatives: 93.26% of Croatian mothers, 87.21% of mothers from BiH, 85.3% of mothers from Srpska, and 80% of Serbian mothers. Over half of participants across all four regions had also heard the opinions that breast milk functions in accordance with the system of supply and demand so that each mother has the exact amount she needs to feed her baby, and that breastfeeding in public is completely acceptable.
However, they also received some very different messages:
-
A mother’s milk can suddenly disappear. (FBiH: 44.19%, Srpska: 32.95%, Croatia: 30.34%, Serbia: 28%)
-
A mother’s milk can “go sour”. (Serbia: 20.5%, other regions, under 6%)
-
Breastfeeding mothers do not, themselves, know whether or not they have enough milk. (Srpska: 37.5%, Serbia: 31%, Croatia: 30.34%, FBiH: 24.42%)

We asked lactivist Tereza Kis Miljkovic where the idea that milk can "go sour" comes from. While she did not know where this longstanding myth originated, because it has seemingly been around forever, she did explain under which circumstances people believe milk can "go sour": if a mother's breasts are engorged, if she eats sour foods, and if she sunbathes.
An approximate 10% of mothers in Serbia, Srpska and Croatia also heard the idea that babies who are smaller than average need formula, while nearly 7% of mothers from FBiH encountered the same view.
Which people in breastfeeding mothers’ personal social circles were most supportive of their choice to nurse their children, then? Partners topped the list in all four regions, with 58% of Serbian breastfeeding mothers reporting that their partners offered them support, along with 31.53% of participants from Srpska, 30.5% of FBiH respondents, and 27.54% of those we surveyed in Croatia. Everywhere, the participants’ own mothers came in second.
It is fascinating to note that only our Serbian and Croatian participants explicitly listed male relatives besides their partners and fathers as being supportive of breastfeeding. While between 2.9% and 6.4% of participants said “everyone” in their social circle was supportive of breastfeeding in Croatia and both parts of Bosnia and Herzegovina, and between 2.4% and 4.43% said “the whole family” was supportive, Serbian respondents also listed their fathers in-law (2.5%), brothers (2%), and even brothers in-law (0.5%) as being supportive. A token 0.48% of Croatian participants likewise said their fathers in law supported their breastfeeding efforts.
One of the parameters by which the general societal acceptance of breastfeeding can be measured is the acceptance of breastfeeding in public. For this reason, we asked our participants who breastfed whether or not they nursed in public, what reactions they encountered if they did, and why they chose not to breastfeed in public if they didn’t.
We received the following responses.
-
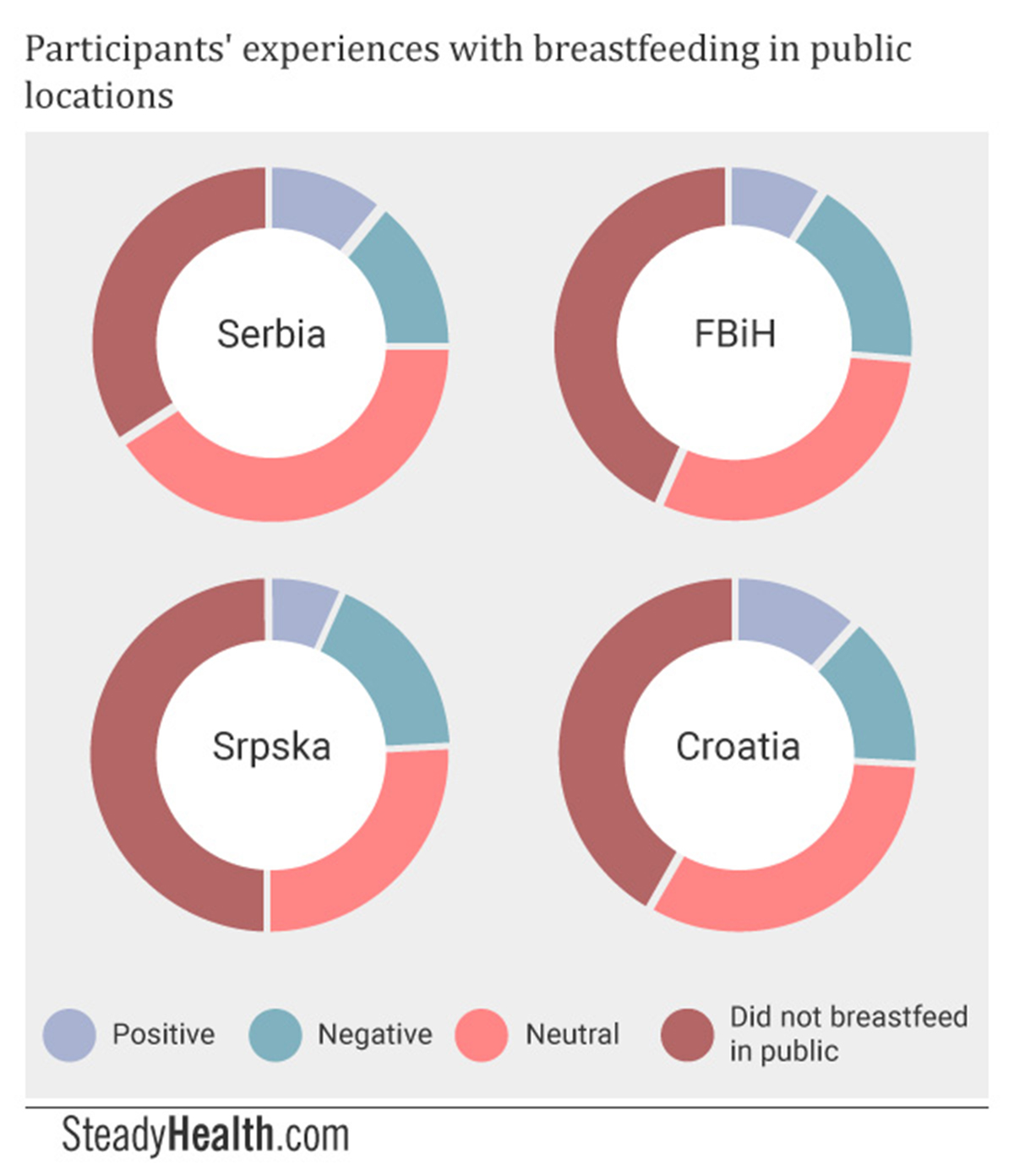
41% of Serbian participants breastfed in public and received neutral reactions, 11% received positive reactions, and 14% was met with negative reactions. 34% did not nurse in public.
-
In BiH, 30.04% encountered neutral reactions to breastfeeding in public, 8.8% positive reactions, 17.8% negative reactions, and 43% never nursed in public locations.
-
25.64% of Srpska respondents was met with neutral reactions, 6.41% with positive reactions, and 17.95% with negative comments and behaviors. A full half of participants from Srpska who otherwise nursed did not do so in public.
-
In Croatia, 32.47% of mothers encountered neither positive nor negative reactions, while 11.69% received positive reactions and 14.29% negative ones. 41.56% did not breastfeed in public.
Some responses from FBiH, for example “I wouldn’t breastfeed in the presence of men, such as my father or brother — I do have some honor”, reveal that cultural beliefs may explain why a lower number of mothers chose to nurse in public there. Likewise, more FBiH respondents added that they used a cover-up if they nursed in public than did women from the other three regions.
At the same time, FBiH participants had some of the bolder responses:
In Serbia, too, we got responses like "I breastfed, but never in public; I believe this to be depraved” and "mothers should manage their time so that there is no need to breastfeed in public." There were mothers who said "I have three kids and mostly got positive comments” and “I think breastfeeding in public is totally accepted here”, along with those who made comments like; "In our country, the trend is still: Oh look, boobs! Let's stare at them!"
While many mothers from Srpska said that they “of course” nursed in public (“Whenever my baby was hungry, in the park, at the doctor’s, on the beach, I don’t care, as long as my baby is happy” and “I didn’t get a single negative comment”), there were also those who were told that “you should do ‘that’ at home”.
In Croatia, mothers’ attitudes ranged from “it is my maternal right to feed my baby whenever and wherever” to “my partner didn’t like me doing that” and one mother was asked: “Why do you want to show your body parts off?”
Mothers’ Beliefs About Breastfeeding
Across the four regions, more than 80% of respondents believed breast milk to be nutritionally superior to formula, while six percent or less thought formula was nutritionally superior.
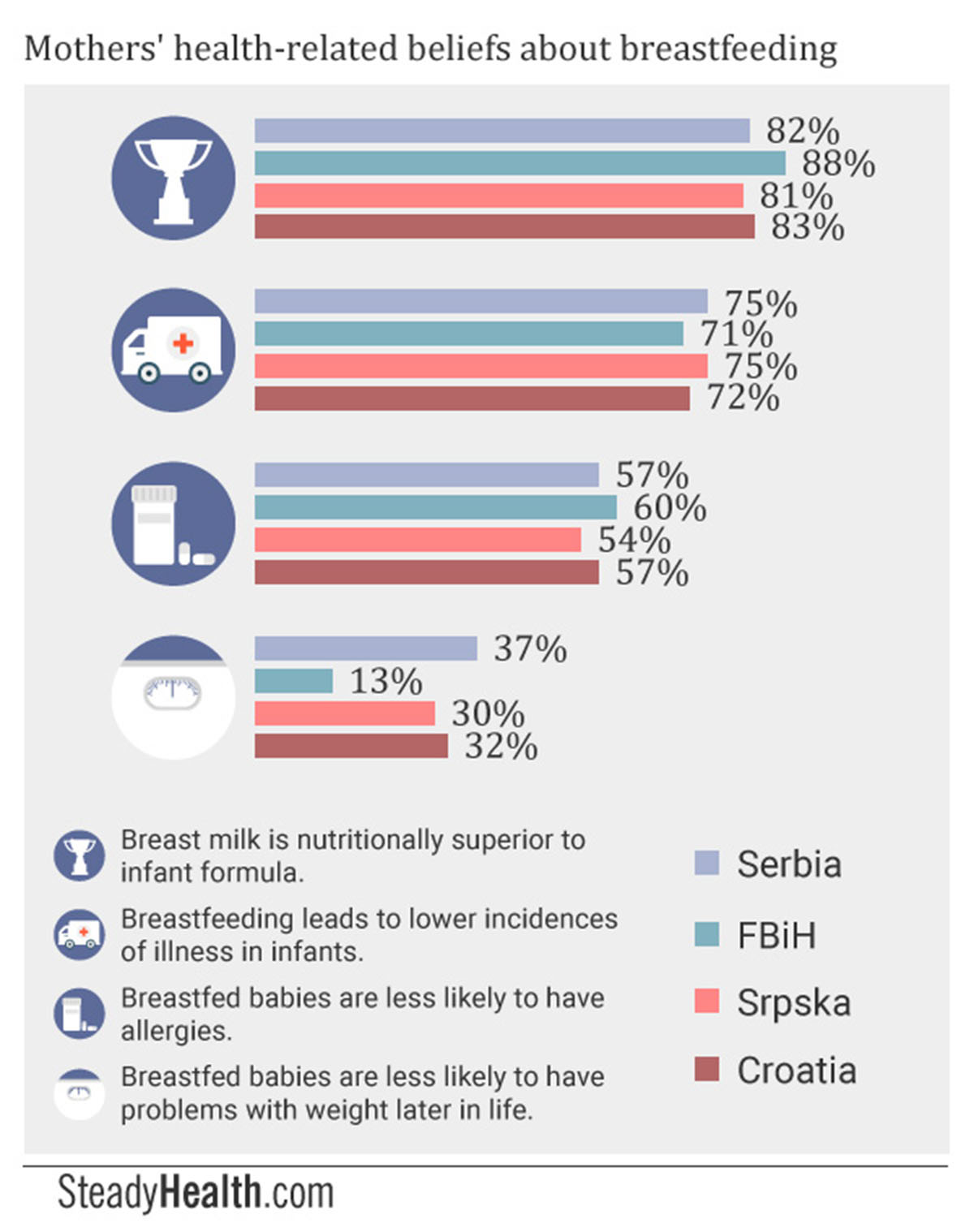
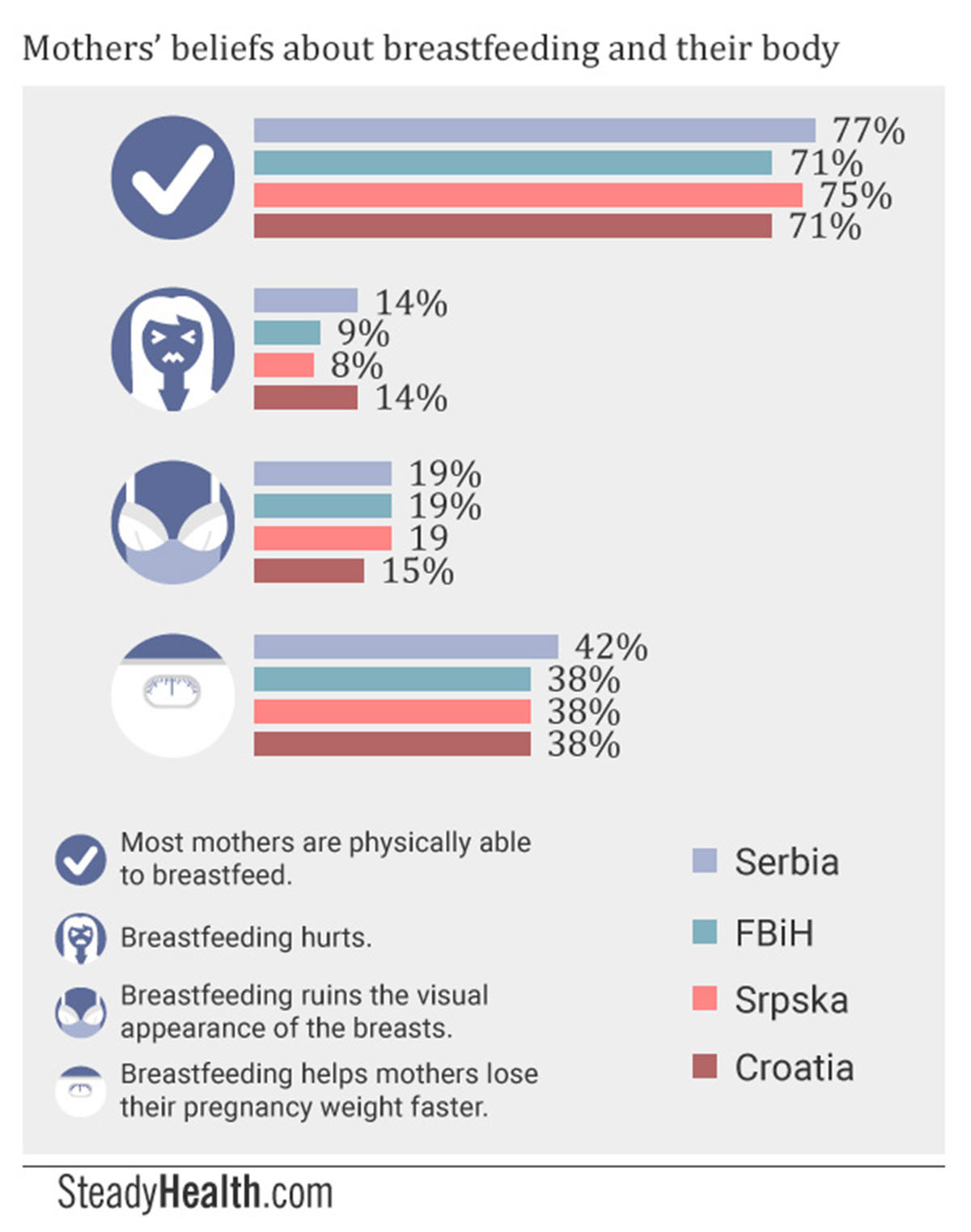
A total of 65% of FBiH participants agreed that nursing offered health benefits to mothers as well, with 62% in Srpska, 58.5% in Serbia, and 54% in Croatia also being aware of this fact. However, 14% each in Croatia and Serbia believed that “breastfeeding hurts”, as well as 9% and 8% in FBiH and Srpska respectively. In addition, 19% of mothers in both parts of Bosnia and Herzegovina and in Serbia held the view that “breastfeeding ruins the visual appearance of the breasts”, something 15% of respondents within Croatia also believed to be true. At the same time, 38% of participants from both parts of Bosnia and Herzegovina and Croatia, and 42% from Serbia, were aware that nursing helps them lose their postpartum weight more quickly.
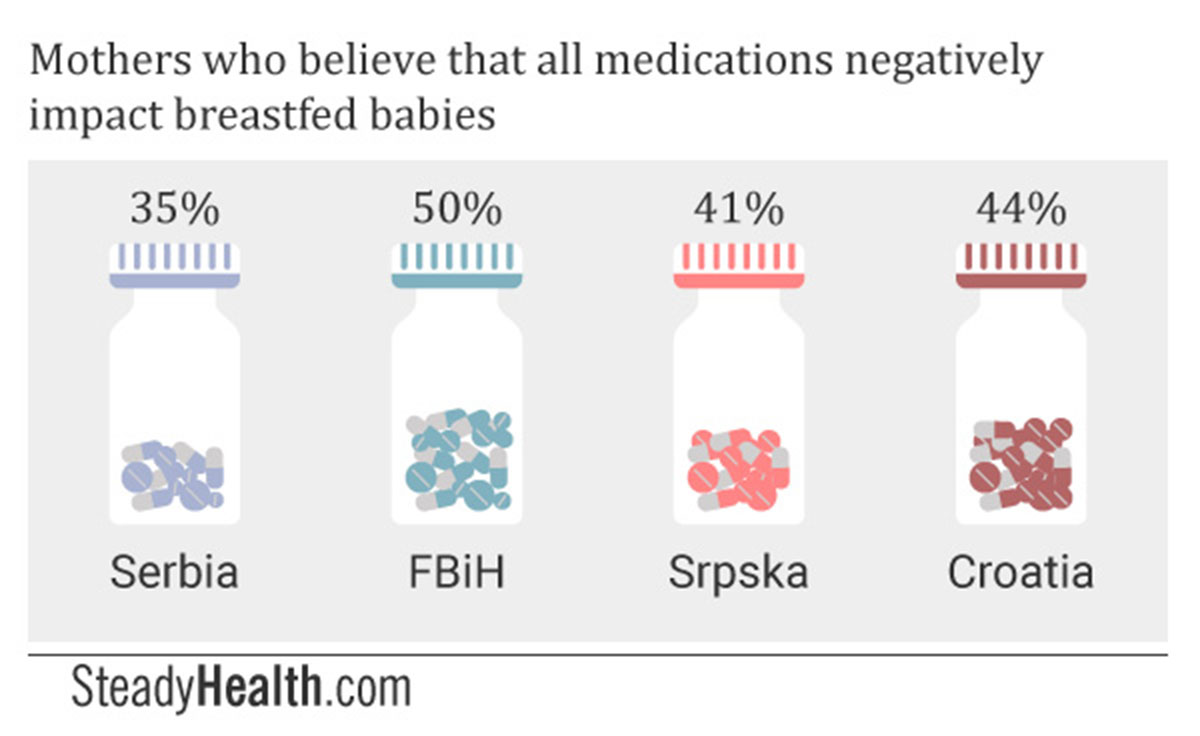
While certain medications do appear in breast milk, and extra care must be taken with premature babies, the widely held belief that all medications a mother takes negatively impact a breastfed baby could both lead mothers who don’t need to stop nursing to feed formula instead, and prevent mothers from accessing adequate healthcare.
Other breastfeeding-related beliefs participants held in large numbers were:
-
Breastfeeding is important, and should be a priority for a mother even when she encounters challenges. (Serbia: 80.5%, FBiH: 78%, Srpska: 76%, Croatia: 74%)
-
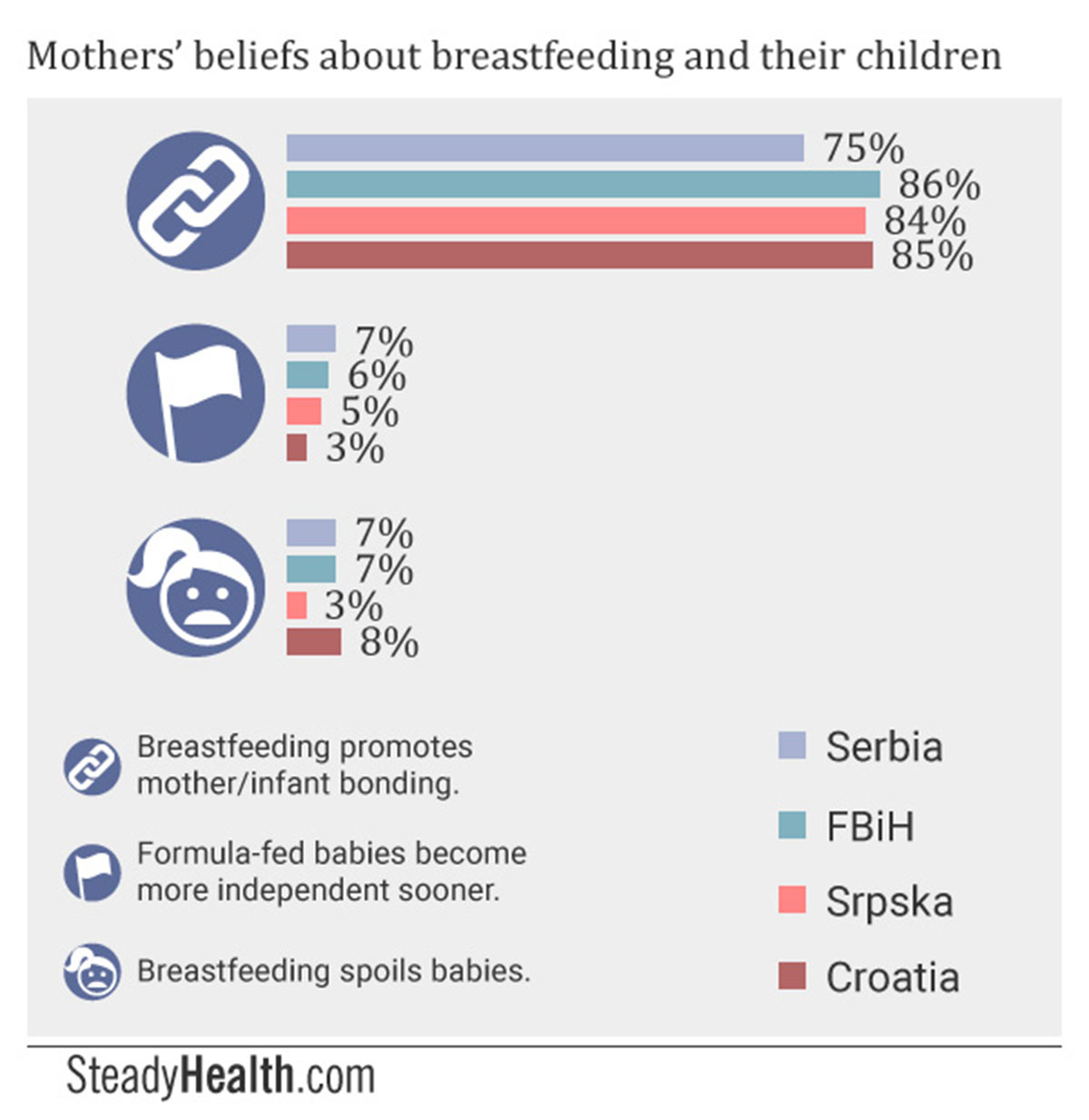
Breastfeeding promotes mother/infant bonding. (Serbia: 74.5%, FBiH: 86%, Srpska: 84%, Croatia: 85%)
-
Mothers should have the legal right to breastfeed in public. (Serbia: 71.5%, FBiH: 59%, Srpska: 61%, Croatia: 56%)
-
Most mothers are physically able to breastfeed. (Serbia: 77%, FBiH: 71%, Srpska: 75%, Croatia: 71%)
-
Many mothers do not have enough milk to feed their babies. (Serbia: 30.5%, FBiH: 31%, Srpska: 27%, Croatia: 35%.)
-
Breastfeeding offers health benefits to mothers and babies, but they are not so significant that negatively judging mothers who choose to formula feed is warranted. (Serbia: 32.5%, FBiH: 37%, Srpska: 35%, Croatia: 44%.)
Less significant numbers than we initially expected answered that they believed mothers should stop breastfeeding without question if a healthcare provider recommends this (less than 9.5% everywhere), that breastfeeding interferes with one’s sex life (less than 7% everywhere), that formula-fed babies display independent behavior earlier than breastfed babies (less than 7% everywhere), and that breastfeeding makes it harder for babies to bond with non-mother caregivers (less than 7% everywhere). Only in Croatia did more than a fifth of mothers indicate that they believed breastfeeding to limit a mother’s opportunity to socialize with others, and only in FBiH did a fifth of respondents reply that mothers who are under stress should not nurse their babies.
Wondering where mothers obtained the beliefs they held about breastfeeding, we asked them both whether they were a member of a breastfeeding support group, and where they primarily gathered information related to parenting.
Serbia had the highest rate of members at 20% of surveyed mothers. In the remaining regions, around 15% reported they were members. We have to note that mothers from both regions of Bosnia mostly added that the support groups they belonged to were online, showing that the internet has become an important medium for accessing support where such infrastructures are not in place locally.
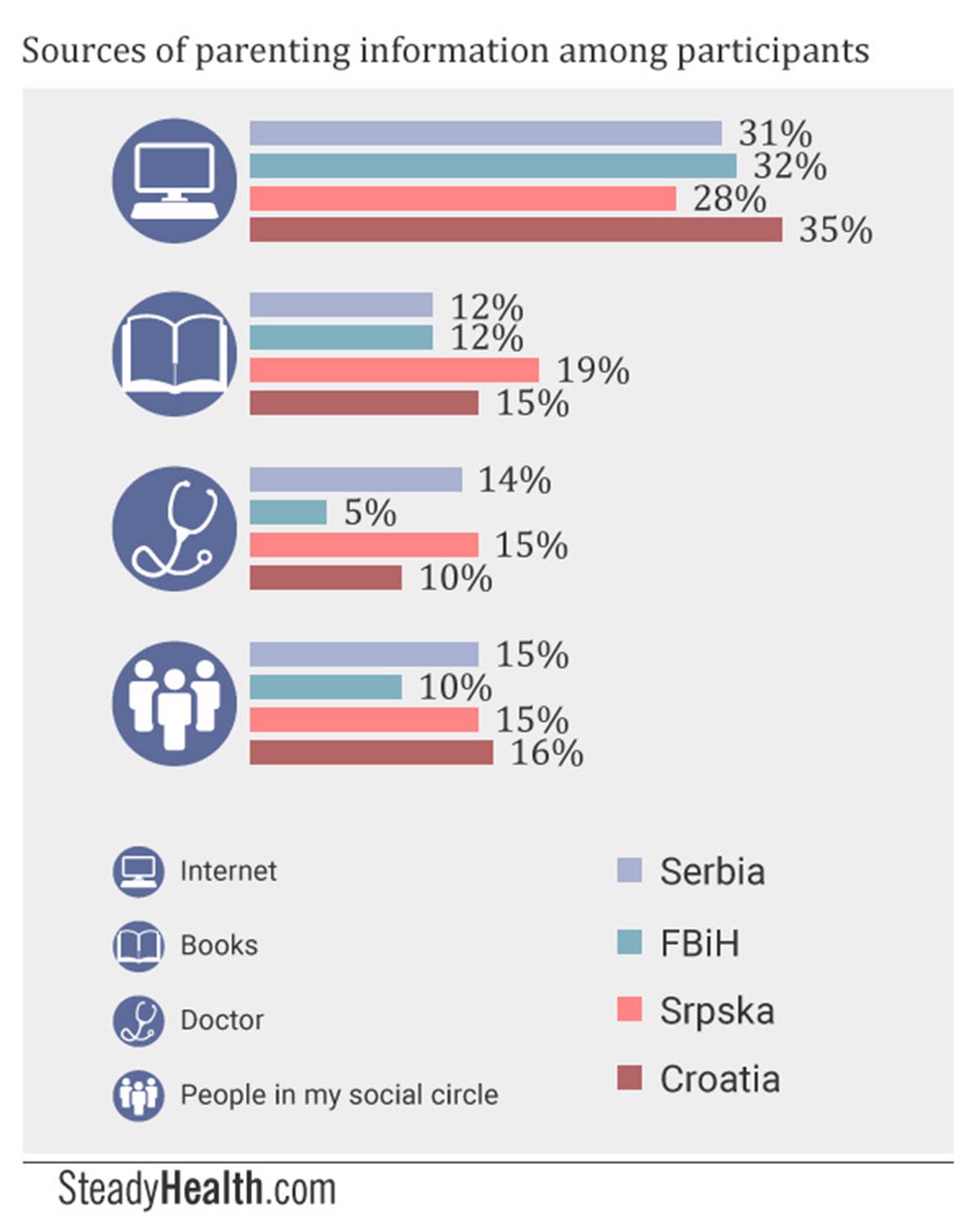
In Serbia, people from participants’ social circles, their doctors, and books were the remaining top three sources of information. In FBiH, books and their own instincts were the most important sources of information besides the internet, with 10% also relying on people they knew and 10% saying they used “any available source of information”. Nearly a fifth of Srpska respondents chose to get their information from books, while their doctor and people from their personal social circle also made up popular sources. In Croatia, meanwhile, mothers sought out books and people they knew, with doctors following closely behind as sources of information.
What Could Be Done To Increase Breastfeeding Rates?
What could be done to increase breastfeeding rates in the four regions we surveyed? We asked participants what they thought would help. The largest number of respondents believed that better education of healthcare providers regarding the benefits of breastfeeding and ways to help mothers succeed at breastfeeding — as well as better education on how to relate to patients in a respectful manner — was the solution in Serbia (35%), FBiH (17.8%) and Srpska (16.46%). Only 4.96% of Croatian respondents answered this way, however.
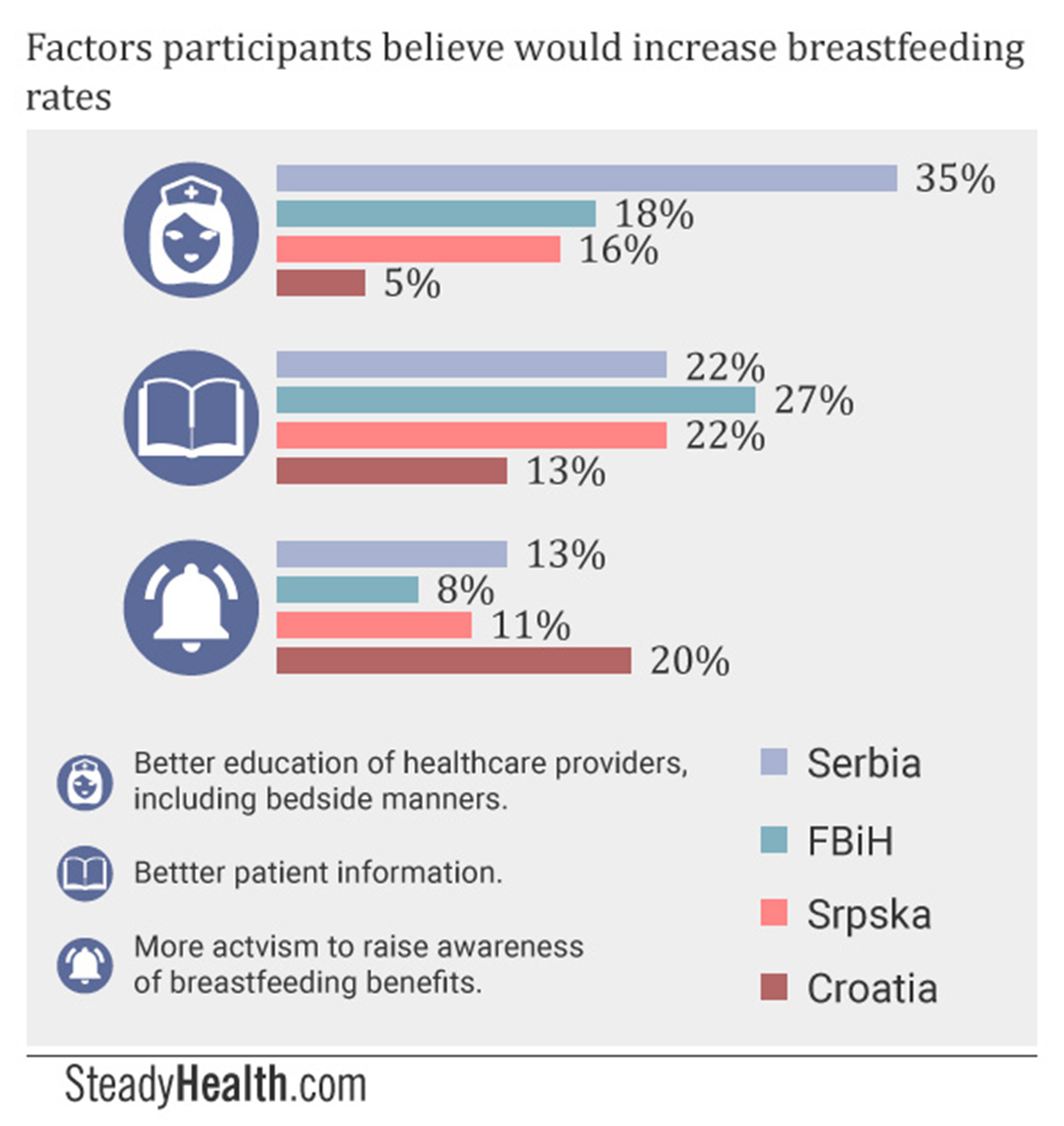
In BiH, meanwhile, 27.4% of mothers believed that better patient information about breastfeeding was the way to increase breastfeeding rates, making this the second most popular answer after better healthcare provider education. Increased social acceptance of breastfeeding was the third most prevalent answer, with 12.5% of mothers believing this to be the solution to low breastfeeding rates in FBiH.
Respondents from Croatia answered very differently: 11.57% replied that the current healthcare system was satisfactory, and that nothing needed to be changed.
Note that not one single person from any of the remaining three regions responded this way, and that there were even those, in these regions, who said that “nothing could possibly be done” or that “everything needs to be changed”.
In Croatia, most respondents rather believed that more media promotion and social activism was the way to increase breastfeeding rates, at 19.83%. Better social acceptance of breastfeeding came in second place as the perceived best way to increase breastfeeding rates, with 16.53% of Croatian respondents answering this way.
Western Balkan Breastfeeding Moms Thwarted By Corruption And Old Wives' Tales: Discussion
Over the course of this project, we had the chance to discuss breastfeeding with numerous mothers from this region. We found that the very notion that a mother would choose, of her own volition, to feed formula rather than breast milk to her baby was outright offensive to many. The reasons for which mothers from this region end up formula-feeding their babies is, as such, much more complex than “a matter of personal choice”.
According to the World Health Organization:
“Poverty, difficulty in accessing health services, social marginalization, obesity (many pregnant women are now overweight or obese), policies in the workplace and the employment market, marketing of breast-milk substitutes, commercial "follow-on" and complementary foods are just some of the reasons for low breastfeeding rates and inequality in the WHO European Region.”
All the countries we surveyed have universal social healthcare systems, and treatment is accessible even to those who lack health insurance. As such, it would not appear that poverty prevents a large number of mothers from accessing healthcare services. Interestingly enough, we also also didn’t find that a significant number of mothers chose to formula feed because they had to return to work and leave their children in the care of others.
The widespread supplementation of breast milk with formula in maternity hospitals, whether the result of financial incentives for healthcare providers or due to cultural attitudes, seemed to have a larger negative impact on breastfeeding rates.
In addition, the prevalent belief that mother’s milk can suddenly disappear and that many mothers simply don’t have enough milk to feed their babies appeared to play a huge role mothers’ decisions to feed formula.
Asking Tereza Kis Miljkovic, a lactivist active across the whole region, and best known for her group "My Breastfeeding Support", which many of our respondents incidentally cited as one they belonged to, about the current situation as well as potential solutions, she answered:
"What percentage of women truly can't breastfeed? It is common knowledge that we're talking about single-digit numbers here, just like in the rest of the world. I can say, with certainty, that the practice of 'supplementing' is incredibly widespread. Those first postpartum days are very important for successful lactation, and we are dealing with missed days, not hours. I can say from experience that this difficult start can play a role, but not the most important role. After mothers and babies leave the hospital, erroneous expectations, misinformation, myths, and fear enter the scene. To every, even the smallest, dilemma, the offered answer is: bottle-feed your baby. This is where the support system fails, and why so many mothers than come to me and ask for help. Balkan mothers don't have any kind of genetic predisposition preventing them from breastfeeding. What they lack is education, support, and a place to turn."
Breastfeeding rates in the region we surveyed are influenced by a complex symphony of lacking knowledge about breastfeeding among healthcare providers, outdated practices in this area, patient perception of a healthcare cadre that is unwilling to help them or lacks time, insufficient patient awareness of the mechanics of breastfeeding, and detrimental society-wide attitudes towards breastfeeding, particularly the notion that many mothers do not have (enough) breast milk. The path towards higher breastfeeding rates can only be be found in addressing these problems.
- Infographics by SteadyHealth.com
- www.euro.who.int/__data/assets/pdf_file/0017/243323/Serbia-WHO-Country-Profile.pdf?ua=1
- www.euro.who.int/__data/assets/pdf_file/0010/243289/Bosnia-and-Herzegovina-WHO-Country-Profile.pdf?ua=1
- www.euro.who.int/__data/assets/pdf_file/0003/243291/Croatia-WHO-Country-Profile.pdf?ua=1
- www.who.int/mediacentre/news/statements/2011/breastfeeding_20110115/en/
- www.euro.who.int/en/health-topics/disease-prevention/nutrition/news/news/2015/08/who-european-region-has-lowest-global-breastfeeding-rates


Your thoughts on this