Arthritis, which is characterized by the inflammation of joints, is a painful and debilitating disorder that is associated with joint stiffness and pain. There are more than a 100 different forms of arthritis, the major categories of which include degenerative arthritis (osteoarthritis), inflammatory arthritis, infectious (septic) arthritis and metabolic arthritis (gout).
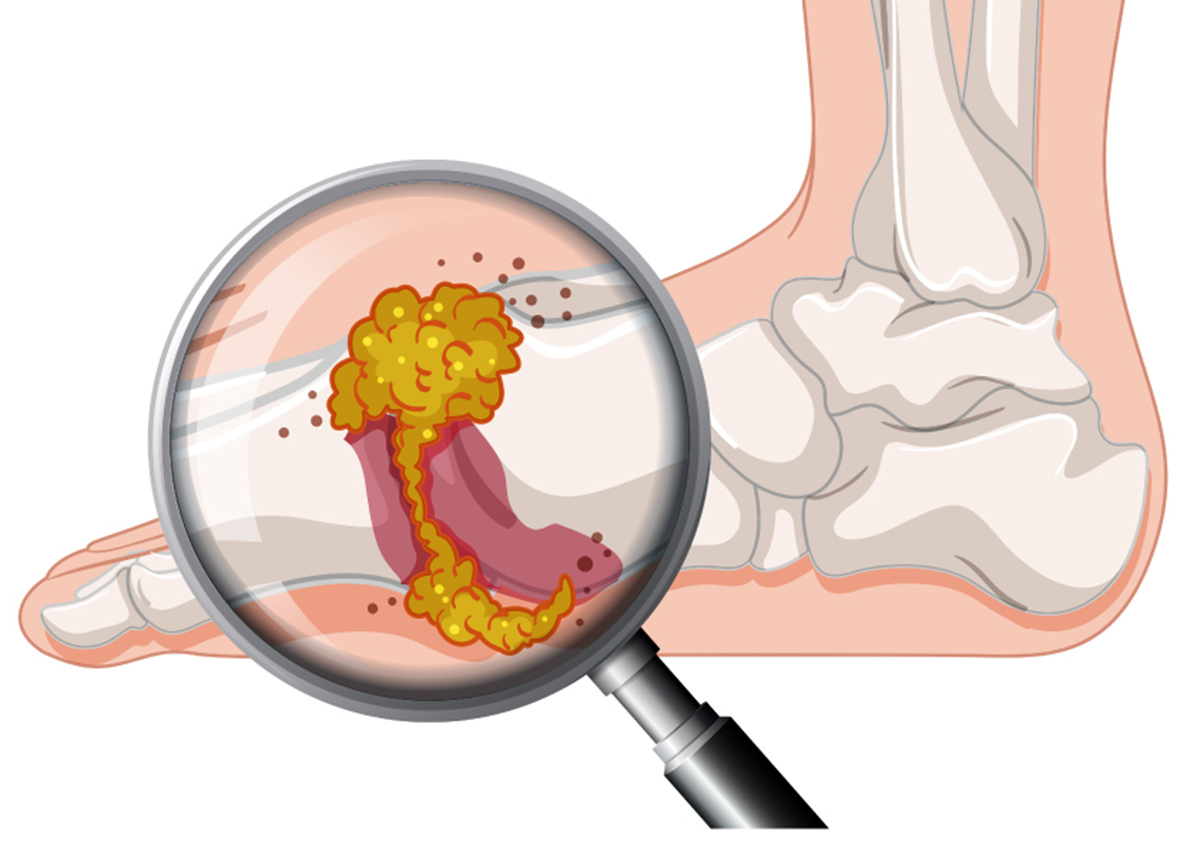
Gout is a type of arthritis that develops due to the presence of sodium urate crystals in your joints. While these crystals can reside there for a long time without causing any problems, they occasionally trigger attacks of gout.
Gout develops due to an impairment in how the body processes or metabolizes a substance called urate. Essentially, urate is removed from the body by the kidneys. Therefore, if the kidneys cannot keep up with the removal of urate, then it continues to build up. Over time, this process leads to the formation of urate crystals in and around your joints.
Causes of gout
As mentioned above, gout occurs in people who have high levels of urate in their blood. While most of the urate in our bodies comes from the breakdown of a substance called purine that naturally occurs in our cells, about a third comes from breakdown of purines that are found in foods and drinks. Gout develops due to a threshold effect, which means that you can have high levels of urate but no crystals until your levels of urate reach a saturation point, which is when you start to develop crystals.
These are the risk factors that can predispose an individual to develop gout:
- Genetics. Certain genes that you inherit from your parents can predispose you to have issues eliminating urate from your body. Hence, family members of patients with gout are more likely to be affected.
- Weight. Patients who are overweight or obese naturally produce more urate at a rate which their kidneys often can’t keep up with.
- Other diseases. High levels of cholesterol and fats in blood, high blood pressure, diabetes and kidney diseases can cause the kidneys to not keep with the rate of elimination of urate, which, in turn, leads to the development of gout.
- Medication. Diuretics, a class of drug, reduce the ability of the kidneys to effectively get rid of urate.
If there is a particular reason that can be identified as causing gout, such as high cholesterol or medication, then the disease is called secondary gout.
However, in most cases, gout is primary which means that is develops due to a combination of multiple factors. In such an instance, a patient will develop gout because they have a kidney disease and are overweight.
For patients who are prone to developing gout, these are the things that can increase the likelihood of having a gout attack:
- Knock or injury
- Disease, such as pneumonia or flu
- Surgery
- Eating and drinking too much alcohol
- Dehydration
Symptoms of gout
The primary symptom of gout is the characteristic symptom associated with arthritis – a painful, red, hot and swollen joint.
Generally, gout appears in the big toe, and attacks occur at night. However, it can also attack other joints including joints in the feet, ankles, knees, elbows, wrists, and fingers.
Other symptoms include:
- The skin that covers the joint can appear and shiny and may start to peel.
- Symptoms develop quickly and are the worst within the first 12 to 24 hours.
- Even light contact with the affected joint is extremely painful (such as having a bedsheet on top or putting on a sock).
- Urate crystals can form small, firm white lumps called tophi, which can be seen under the skin and outside the joint. They can also sometimes secrete a pus-like fluid.
Diagnosis: How do doctors diagnose gout?
If your doctor suspects you have gout, then he or she will examine the joint, question you about details regarding the symptoms, and will send you for a series of tests. A diagnosis is made by combining information from family and personal medical history, physical and examination and results from a number of different tests including:
- Blood tests to measure the levels of urate in your blood. If it is above the threshold point, then that can point to a diagnosis of gout, but can’t confirm it. Furthermore, some patients with gout may actually may normal levels of urate in their blood during an attack.
- Imaging tests such as X-rays, which can help evaluate the level of joint damage. Ultrasounds can also be used to detect signs of gout, and can add information if the physician is uncertain about the diagnosis.
- Examination of the synovial fluid, which is a fluid that surround the joints. The synovial fluid is extracted through a needle and examined under a microscope to help confirm the presence of urate crystals.
Treatment: How is gout managed?
There are two major ways of treating gout:
- Treating the patient during an attack of inflammation, when one or more joints are extremely inflamed and painful. The two most common drugs used for treating these attack are non-steroidal inflammatory drugs (NSAIDs), such as such as aspirin and naproxen, and colchicine (which helps reduce inflammation caused by the crystals in the joint lining).
- Ongoing treatment to help lower levels of urate in your blood and eliminate urate crystals. For this type of treatment, you can take specific medication every day to help lower inflammation or bring down levels of urate. Allopurinol is the most common urate-lowering drug, but NSAIDs and colchicine can also be taken every day. Febuxostat is another recently developed urate-lowering drug.
- Puig, Juan G., et al. "Female gout: clinical spectrum and uric acid metabolism." Archives of internal medicine 151.4 (1991): 726-732.
- Magliano, Malgorzata. "Obesity and arthritis." Menopause international 14.4 (2008): 149-154
- Falasca, Gerald F. "Metabolic diseases: gout." Clinics in dermatology 24.6 (2006): 498-508.
- Photo courtesy of SteadyHealth.com


Your thoughts on this