Table of Contents
An open discectomy is the most common surgical treatment for ruptured or herniated discs of the lumbar spine. This surgery is used to remove a part of the damaged disc which is relieving the pressure on the nerve tissue and alleviating the pain.
The surgery involves:
- A small incision in the skin over the spine
- The removal of some ligament and bone material
- The removal of some of the disc material.
Doctors have been performing open discectomy procedures for nearly 80 years. Modern medical technologies like magnetic resonance imaging (MRI) and computerized tomography (CT) have allowed medical professionals to refine the procedure further.
This operation has an excellent success rate of 80 to 90 percent. Studies have also shown that discectomy operations are more successful in people with radicular pain than in those with low back pain.
Pathophysiology of the condition
Vertebral discs are cushioning and connecting materials that lie between the bones of the spine. When the outer wall of this disc becomes weakened through age or injury, it may tear and eventually bulge out. This is called disc herniation, disc prolapse, or a slipped or bulging disc.
Once the inner disc extends out it can press sensitive nerve tissue in the spine. This then causes weakness, tingling, or pain in the back area and into one or both legs. Herniated disks can affect your ability to perform everyday tasks and can cause severe pain. Although the pain is simply unbearable at times, herniated disks aren't likely to result in paralysis.
Proper indications for a discectomy
Not all patients with herniated discs are candidates for the open discectomy procedure. This operation is usually the option of last resort if other possible treatments such as rest, physical therapy, anti-inflammatory medications, and epidural injections didn’t offer relief or improve functionality.
Before the operation, the doctor may order diagnostic tests, such as X-rays, MRI or a CT scan, to verify the source of the pain. If a diagnosis of a herniated disc is confirmed, an open discectomy may be recommended.
Open disectomy: How is it done?
This operation is performed under general anesthesia.
The surgeon makes a one-inch incision in the skin over the affected area and removes the muscle tissue above the bone.
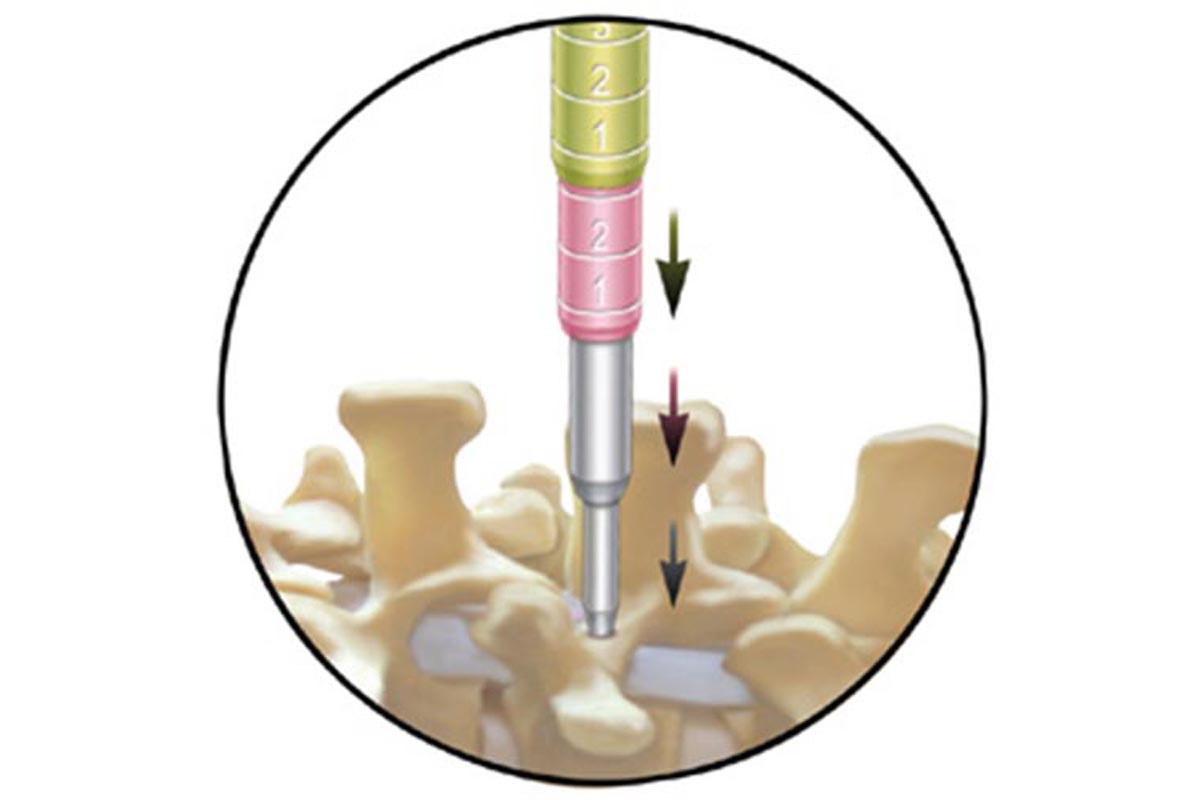
In some cases, bone and ligaments may also need to be removed for the surgeon to be able to visualize the bulging disc without damaging the nerve tissue. This is called a laminectomy.
During a laminotomy a portion of lamina is removed to relieve pressure on a nerve or allow the surgeon access to a disk that's pressing on a nerve. When the surgeon finishes all the preoperative preparations, the section of the disc that is protruding from the disc wall will be removed. This should relieve all the symptoms and allow the patient to enjoy a higher quality of life. No implants and no artificial material is used to replace the disc tissue that is removed.
- www.spine.org
- en.wikipedia.org/wiki/Anterior_cervical_discectomy_and_fusion
- www.spineuniverse.com
- image: www.texasspinecenter.com

