Researchers have used the DiaRem score to predict whether patients with type 2 diabetes could be cured with bariatric surgery.
The study
Data was analyzed from medical health records of over 400 patients who were diagnosed with type 2 diabetes and who had undergone a Roux-and-Y gastric bypass surgery (RYGBS). The criteria that needed to be met was that the records had to be at least 5 years old and patients' data up to 8 years after the operation was analyzed. These records came from patients who had participated in the original DiaRem study.
The aim of the study was to look at whether the DiaRem score could predict complete remission of type 2 diabetes, which was defined as the return of normal glucose values and no treatment being used for a year, and if the score could predict a cure for the condition, which was defined as complete remission for 5 years.
The findings
The following conclusion were made:
- 24% of the patients had partial remission which lasted at least 1 year.
- 35% of the patients had 1 or more years of complete remission.
- 25% had a prolonged partial remission.
- 20% of patients were cured of type 2 diabetes.
- In patients who were achieving decreased remission, the DiaRem score increased. This was true for any length of remission.
The clinical significance
The conclusive findings were that bariatric surgery not only put type 2 diabetes into remission, but also cured it in a percentage of patients. The patients who were more likely to experience these benefits were those with lower DiaRem scores.
This would indicate that patients seen in a clinical setup who were diagnosed with type 2 diabetes, and who had low DiaRem scores, could benefit from bariatric surgery. The sample data of this study was reasonably low, therefore further research on larger population groups has been suggested by the research team.
The biggest benefit of such a procedure, in patients with type 2 diabetes, is that it would improve their quality of life by reducing the risk of developing complications.
READ Doctors May Have Developed a New No-Knife Surgery for Gastric Bypass
Complication of diabetes
The following are complications associated with diabetes.
- Nerve damage - this occurs due to injury to the small vessels carrying blood to the nerves. When the blood flow to these nerves are compromised, then the nerves start to become damaged.
- Cardiovascular disease - such as heart attacks and strokes.
- Eye issues - such as cataracts and glaucoma.
- Kidney damage - due to damage by excess glucose to the filtering system of the kidneys.
- Foot-related issues - such as decreased sensation in the feet and slowed healing of wounds.
- Skin conditions - such as fungal and bacterial infections.
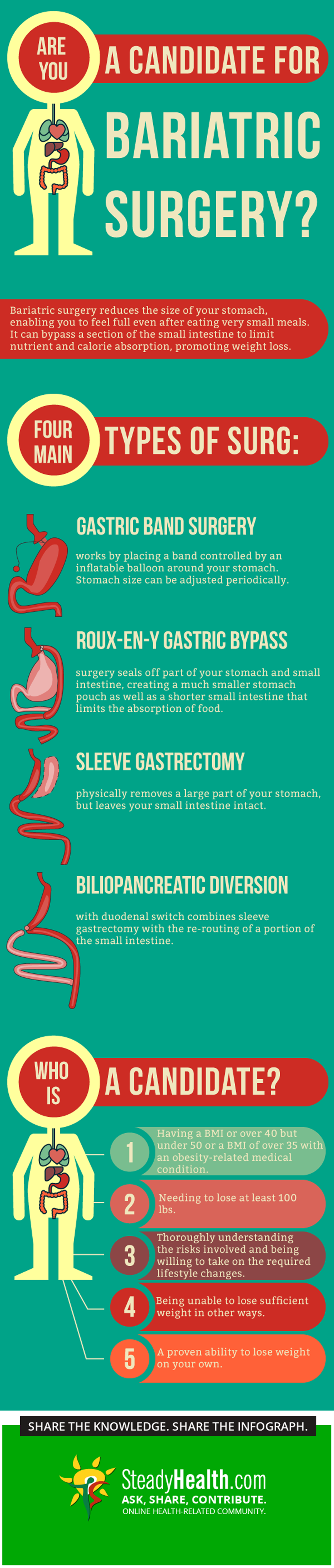
Bariatric Surgery: Are You A Candidate?
This procedure is performed by altering the digestive tract of patients and is being done as a weight-loss strategy by limiting how much a person can eat. There are many types of surgeries done to aid in weight loss and these are collectively known as bariatric surgery. Of these surgeries, the most commonly performed procedure is a gastric bypass as it's associated with fewer side-effects than other procedures.
Indications
Gastric bypass surgery is performed in order to help patients lose weight and therefore reduce their risk of developing life-threatening issues such as:
- Heart diseases such as strokes and heart attacks.
- Hypertension (high blood pressure).
- Type 2 diabetes.
- Severe obstructive sleep apnoea.
- Gastro-oesophageal reflux disease.
This procedure is limited to those patients who have tried other methods to lose weight but weren't successful. Other criteria which would need to be fulfilled by patients in order to have this procedure done are:
- Being morbidly obese - having a body mass index (BMI) of 40 or higher.
- Having a BMI of between 35-40 and being diagnosed with a serious weight-related condition such as those mentioned above.
- Having a BMI of between 30-35 and a life-threatening weight-related issue.
Types of procedures
- Roux-and-Y - this is the most common gastric bypass procedure, and is typically irreversible as the capacity of the stomach is reduced by sealing the top of the stomach off from the rest. The small intestine is then cut and attached to this new pouch.
- Biliopancreatic diversion with duodenal switch - here, 80% of the stomach is removed and most of the small intestine is bypassed.
- Laparoscopic adjustable gastric binding (LAGB) - an inflatable band is placed over the upper-most part of the stomach to reduce its capacity.
- Vertical banded gastroplasty - the stomach is divided into 2 parts restricting the amount of food which can be eaten. Major weight loss doesn't occur here and is therefore not such a popular option.
- Sleeve gastrectomy - this is a newer procedure where the stomach is shaped into a tube so as to absorb less calories.
READ Treat Obesity With Gastric Bypass Surgery
Risks
Gastric bypass and other weight-loss surgeries can be associated with certain risks. They can include the following issues:
- Post-operative infection - if this occurs, it would be noticed on the 3rd day after surgery.
- Excessive bleeding - during or after the procedure.
- Thromboembolic events - the risk of developing a deep venous thrombosis/clot in the lower legs increases in obese patients. The risk is also increased after any surgery. Preventative measure would need to be followed by the doctors involved as a clot in the legs can break off and lodge in the pulmonary arteries. This is called an embolus and results in a reduced blood flow to the lungs which could be fatal.
- Adverse reaction to anaestheisa - also, during of even after the procedure.
- Leaks in the gastrointestinal system - as a direct issue related to the surgery.
- Respiratory related issues - such as adult respiratory distress syndrome (ARDS) or the mentioned pulmonary embolus.
Long-term complications
These would depend on the type of surgery which is done and may include the following issues:
- Dumping syndrome - occurs due to certain parts of the stomach being removed and is associated with nausea, vomiting and diarrhoea.
- Formation of gallstones.
- Bowel obstruction - mostly due to adhesion formation in the operated areas.
- Stomach perforation.
- Stomach or duodenal ulcer formation.
- Hernias - usually involving the surgical sites.
- Hypoglycaemia (low blood sugar).
- Malnutrition - due to malabsorption as a result of specific parts of the small intestine being removed. The most common deficiencies are those of vitamin B and iron.
- www.medicalbrief.co.za/archives/diarem-predicts-cure-of-type-2-diabetes-through-surgery/
- www.mayoclinic.org/diseases-conditions/diabetes/basics/complications/con-20033091
- www.mayoclinic.org/tests-procedures/bariatric-surgery/basics/definition/prc-20019138
- Photo courtesy of
- Photo courtesy of
- Photo courtesy of


Your thoughts on this