A routine blood test is often prescribed for most healthy people to check or screen for any disorder that has not been previously detected. For example, you may have an elevated blood sugar level without knowing it because your symptoms are mild or you feel just fine. You may be anemic or have a low hemoglobin count, which you find out only after a routine blood test. These screening tests may help detect the presence of a potential health problem before it becomes symptomatic or worse, especially in those who are at risk. People may also get routine blood exams to check if their state of health has improved after receiving treatment for a previously diagnosed disorder.
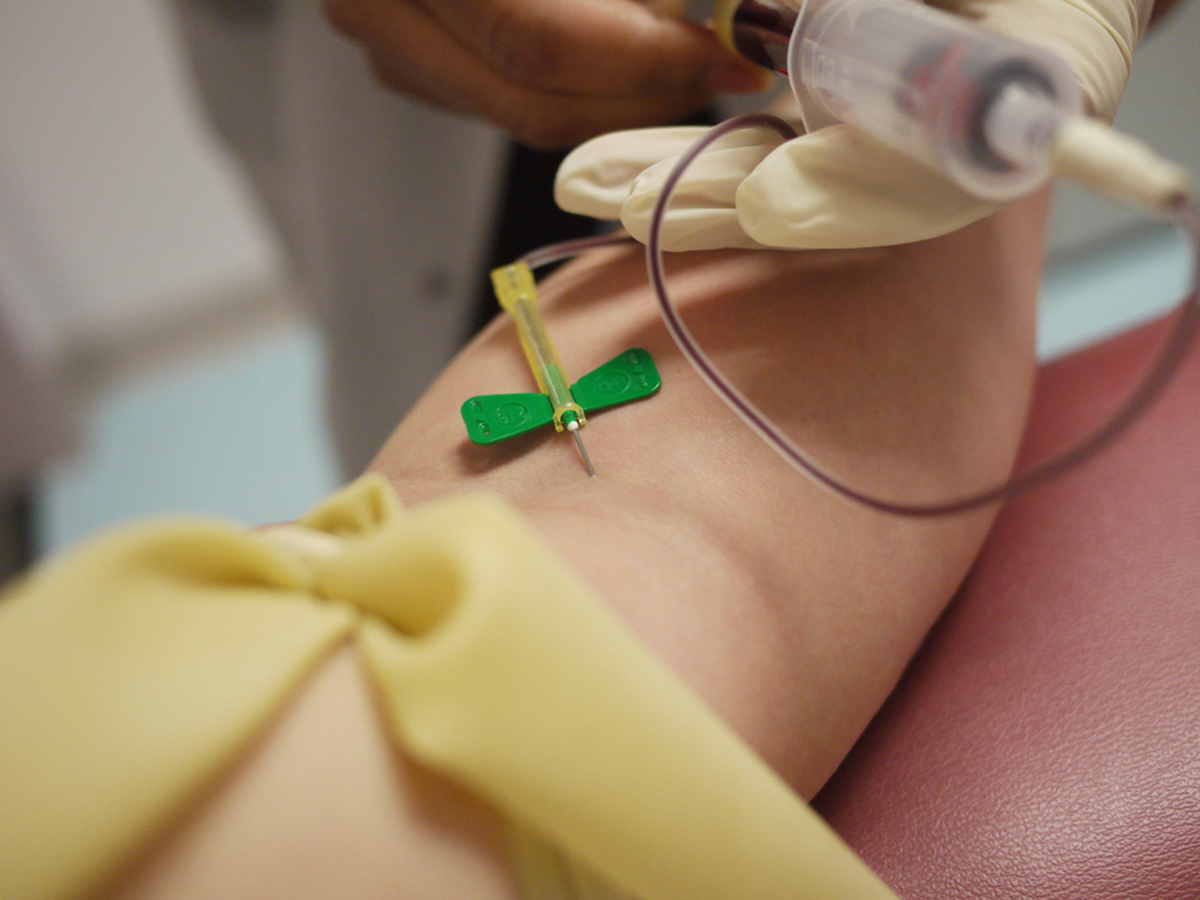
Routine blood tests usually include a complete blood count (CBC), a blood chemistry test (also called Basic Metabolic Panel), and a blood lipid profile. Requests for particular blood tests may vary for pregnant women, people who are 50 years old and above or young children. A complete blood count usually measures the number of red blood cells, white blood cells, and platelets, and the amount of hemoglobin (an oxygen-carrier) in the blood. Your hematocrit will help determine whether you are dehydrated, anemic, or if you have bone marrow disorder. A routine blood chemistry test usually examines your blood glucose (sugar) levels, calcium, electrolytes, and kidney function (BUN and creatinine). Your blood lipid profile or lipoprotein panel measures your total cholesterol as well as your bad (LDL), good (HDL), and triglyceride levels. Additional tests may be ordered to check if you are at risk for certain diseases, such as heart disease (blood clotting tests) or liver disease (liver function test).
Fasting Instructions
Most patients are instructed to fast to prepare for a routine blood test. They are usually told to stop eating or drinking anything except water 8-12 hours before getting their blood test, particularly if they are to undergo testing for fasting blood sugar (FBS) levels and/or lipid levels. Recommendations for fasting before blood exams were originally made to reduce variability and to achieve consistency in the patient’s metabolic state at the time of blood extraction. It is believed that food and beverages contain nutrients that are absorbed into the blood stream and could affect certain factors measured in the blood tests, such as your glucose or lipid (cholesterol and triglyceride) levels.
Many patients, however, have difficulty keeping their fasting state. Some are inclined to forget or even cheat, which may lead to postponing or repeating their tests. Poor patient compliance may also lead some people to avoid getting tested. Furthermore, some doctors also sympathize with their patients, whom they feel, are placed on unnecessary starvation.
See Also: Your Blood Never Lies: You Can Use Simple Laboratory Tests to Make Informed Health Decisions
Several studies have recently suggested that patients may not be required to fast before getting some of their lab exams, particularly their lipid profiles. Of course, a fasting blood sugar (FBS) test requires at least an eight-hour fast, since the test wants to find out how much sugar is left in the blood even when a person has not eaten for several hours. But this is not the same for blood cholesterol exams. Researchers found that there is a minimal difference in the results of lipid profiles between the fasting state and the non-fasting state, which makes the obligatory fasting unnecessary for these tests.
Fasting Is No Longer Necessary For A Lipid Panel
A lipid panel gives you a profile of how much cholesterol you have in the blood – this includes HDL or good cholesterol, LDL or bad cholesterol, total cholesterol and triglycerides. This test is often done to evaluate one’s risk for developing heart disease. High cholesterol is a significant risk factor for developing atherosclerosis, a condition where cholesterol builds up inside the arteries, thus reducing effective blood circulation. When the arteries of the heart (the coronary arteries) are affected, your likelihood for developing heart disease and your risk of having a heart attack are increased. The blood test is therefore routinely recommended for people who are more than 50 years old and for others who may have other risk factors such as a strong family history of heart disease. It may also be done as a guide to treatment for those who are receiving cholesterol-lowering medications (statins).
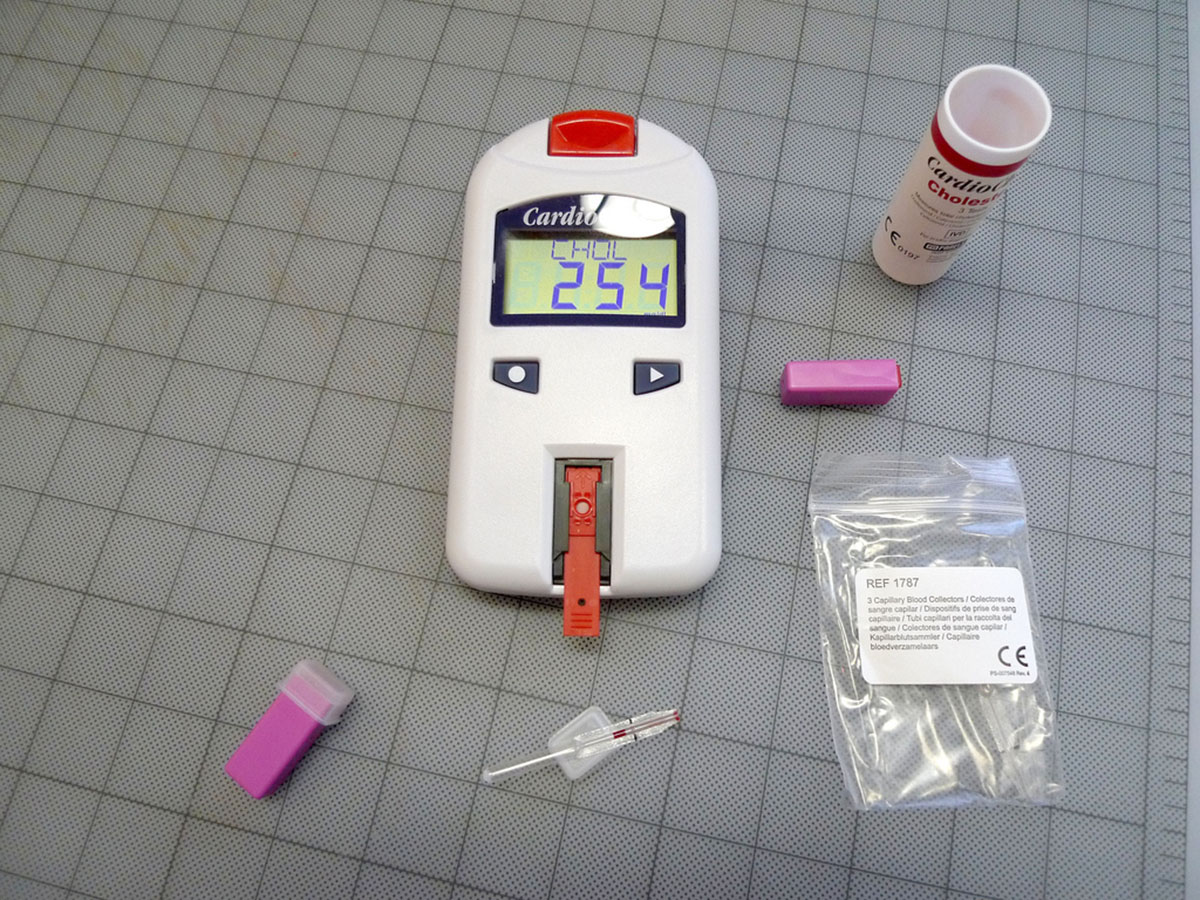
Inasmuch as many people find it difficult to fast for 8 to 12 hours, some doctors also feel that starving their patients may be unnecessary. Experts now believe that requiring patients to fast before taking a lipid panel test is pointless, if not bad medicine. One study, which involved more than 200, 000 participants, found that variations in fasting time had no significant association with lipid levels. Another study, which compared lipid levels in the fasting and non-fasting states, found that lipid profiles change minimally after normal food intake. The participants were followed for 14 years and researchers found that non-fasting lipid profiles were able to predict increased risk of heart attack and stroke. These studies suggest that there is no benefit from asking patients to starve for several hours before taking a lipid profile because there would be not much difference if the test were taken after they had just eaten a normal meal.
Many experts agree that it is more practical to remove the burden of fasting to encourage more people to get tested for blood cholesterol levels. Sripal Bangalore, a cardiologist, author, and associate professor at the New York University Langone Medical Center comments that since people are usually in the non-fasting state, it makes more sense to measure their blood cholesterol levels in their natural state, when they are exposed to bad cholesterol.
See Also: Big Breakfasts And Diabetes: Can A Big Breakfast Improve Blood Sugar Control?
Easing the requirement for fasting does not mean that bingeing before a blood test is taken is acceptable. All that is being said by doctors who allow a non-fasting state is that one may take their normal meals without being concerned that their test results will be affected. Studies have found that the difference in results may be minimal (up to 10% difference). It must be noted, too, that these recommendations do not hold true for all blood tests, such as FBS. It would therefore be safer to follow your physician’s instructions regarding your preparation for taking a blood test.
- Medpage Today. Is Lipid Management a Sham? http://www.medpagetoday.com/Cardiology/Prevention/48427 Circulation. Fasting and Nonfasting Lipid Levels. http://circ.ahajournals.org/content/118/20/2047.full JAMA. Fasting Time and Lipid Levels in a Community-Based Population. http://archinte.jamanetwork.com/article.aspx?articleid=1391022 Circulation. Prognostic Value of Fasting vs. Non-Fasting Low Density Lipoprotein Cholesterol Levels on Long-term Mortality: Insight from the National Health and Nutrition Survey III (NHANES-III). http://circ.ahajournals.org/content/early/2014/07/10/CIRCULATIONAHA.114.010001.abstract NY Daily News. Hate fasting before a blood test? Soon, you might not have to: study. http://www.nydailynews.com/life-style/health/fasting-blood-test-not-best-study-article-1.1863653 NIH. Types of Blood Tests. http://www.nhlbi.nih.gov/health/health-topics/topics/bdt/typesPhoto courtesy of Thirteen Of Clubs via Flickr: www.flickr.com/photos/thirteenofclubs/5457366051
- Photo courtesy of Juhansonin via Flickr: www.flickr.com/photos/juhansonin/5300977759
- www.medpagetoday.com
- circ.ahajournals.org
- archinte.jamanetwork.com
- www.nydailynews.com
- www.nhlbi.nih.gov

