It was not long after the introduction of first antibiotic agents that scientists started noticing the existence of certain resistant organisms. The term “resistance” means that the bacterial cells continue to replicate in the presence of a given amount of a drug to which they are normally susceptible to. This resistance has two important consequences: either the amount of antibiotic needed to eliminate the bacterial cells needs to be increased, or the antibiotic is rendered totally ineffective. The latter is of course more worrisome and it is a serious issue of modern-day society.
Mechanisms of bacterial resistance to antibiotics
Drug resistance typically arises through mechanisms that block the interaction of a drug and its target. The target is, usually, a protein in the bacteria which is absent in human cells. Possible mechanisms of resistance include genetic mutations of the target, enzymatic deactivation of the drug by bacteria, or loss of an enzyme required to activate an antibiotic. They also include mechanisms that prevent a drug from reaching the target, for example, drug export away from the bacterial cell by efflux pumps. or changes that reduce the cell’s permeability of the drug.
Drug tolerance and drug resistance are not the same things
Drug tolerance is another situation, where bacterial cells survive in the presence of a certain concentration of antibiotic but do not continue replicating. Tolerance is associated with a myriad of alterations that lead to dormancy, persistence or cellular changes in bacteria. Let’s look at some of these mechanisms.
Bacterial cells can become dormant
Dormancy is a state characterized by a delicate balance between slow cell growth and death, in which the cell presents with metabolic quiescence. Certain bacterial populations enter this state naturally when they experience situations of limited nutrients.
This type of inactivation is very interesting, especially because there is antibiotics whose effectiveness depends on cellular activity. For example, slowed growth confers tolerance to the cell wall-acting β-lactams (such as antibiotics of penicillin class) due to a decreased need for cell wall synthesis. Similarly, quinolones – which target an enzyme topoisomerase II in bacteria and damage bacterial chromosome – generally require high cellular activity in order to kill bacteria.
See Also: Helicobacter: The Bacteria that Cause Ulcers
Some bacterial species have diverse population with different sensitivity to drugs
Asymmetric growth and division are two other, more sophisticated, processes of bacterial persistence. Such a mechanism has already been described in mycobacteria by a group of researchers from Boston. Mycobacteria are rod-shaped bacteria that elongate from their poles. Within the same clonal population of mycobacteria, there is diversity in the elongation rate because mycobacteria grow asymmetrically, in an uncommon, unipolar fashion. This means that, from the same mother cell, originate daughter cells that inherit an older pole and daughter cells that inherit a younger pole. The former grows faster than the latter, originating physiologically distinct sub-populations that are differentially susceptible to clinically important classes of antibiotics. More specifically, faster growing cells are more susceptible to cell wall-acting antibiotics, while slower growing cells, termed alternators, are more susceptible to other class of drugs called transcription-targeting drugs.
Bacteria Possess Multiple Mechanisms Of Drug Resistance
Mechanisms of actual drug resistance are multiple, but they essentially work by preventing the interaction of the molecules of the antibiotic with its targets in the bacterial cell. Their origin is generally genetic and can result from changes to the bacteria’s own chromosomal DNA or from the acquisition of external DNA segments (e.g. plasmids). Some of the main mechanisms of drug resistance are:

- Enzymatic inhibition: beta-lactam antibiotics (such as penicillin) act on the penicillin-binding proteins (PBPs) located in the bacterial cell wall. These proteins catalyze the synthesis of specific compounds, peptidoglycans, that form the cell wall of bacteria. The most common resistance mechanism to beta-lactam antibiotics is mediated by beta-lactamase enzymes, destroys the molecules of antibiotic. Gram-positive bacteria, such as the Staphylococcus species, excrete the beta-lactamase enzyme in such a way that it inactivates the antibiotic before it can enter the cell.
- Changes to the antibiotic’s target: antibiotics from the groups of macrolides, lincosamides, and aminoglycosides interact with a ribosomal subunit to destabilize protein synthesis. Protein synthesis is performed by specialized cellular machineries – ribosomes. Ribosomes consist of multiple components. Resistance to the macrolides and lincosamides results from the mutations in some of these components that lead to a slightly changed structure unrecognizable to the drug.
- Changes in membrane permeability and antibiotic efflux: the exchange of molecules between bacterial cell and the environment is possible because of the presence of outer membrane proteins (Omps), through which different molecules are transported. These proteins, called porins, are found in the external membrane of gram-negative bacteria. A larger channel porin, such as OmpF, can be substituted for OmpC, which has a smaller diameter. This substitution prevents the entry of larger molecules, such as antibiotic carbenicillin. Another resistance mechanism is the efflux (pumping out) of the antibiotic through the cell membrane to diminish the concentration of the drug inside the cell and prevent it from reaching the target site. Antibiotic efflux occurs with tetracycline, erythromycin, and the fluoroquinolones.
Connection between persistent infections and antibiotic resistance
Although the circumstances and the mechanisms of functioning are different, it is not impossible for persistence and resistance to be connected. The discovery that cellular activity and division can occur during persistence raises the possibility that persistent organisms function as intermediaries in the process of developing the heritable drug resistance. Residual cell division combined with active survival mechanisms could support or even enhance the development of heritable genetic changes, because many of the same stress-response programs important for the generation and survival of persistent bacteria can also accelerate mutations and changes in bacterial genes.
See Also: CDC Warns Of Potential Catastrophe Of Antibiotic Resistance
When an infection becomes persistent, it often signifies that the pathogen causing the infection is able to evade the body's natural defenses or therapeutic interventions over extended periods. Here are some connections between the two:
-
Inadequate Antibiotic Courses: Incomplete or inadequate courses of antibiotics can leave some bacteria alive, potentially allowing them to develop mechanisms to resist the effects of the antibiotic. These surviving bacteria can then multiply, leading to a resurgence of the infection, but now with antibiotic-resistant properties.
-
Overuse of Antibiotics: The over-prescription of antibiotics for viral infections or other conditions they can't treat means that bacteria are exposed to these drugs more frequently. This heightened exposure provides more opportunities for bacteria to evolve resistance mechanisms.
-
Biofilms: Some bacteria can form biofilms, which are complex communities of microorganisms that adhere to surfaces and are embedded in a matrix of extracellular polymeric substances. Within these biofilms, bacteria are protected from antibiotics and can persist in a dormant state, leading to chronic infections. When they are reactivated, they can be more resistant to treatment.
-
Horizontal Gene Transfer: Bacteria have the ability to exchange genetic material through processes like conjugation, transduction, and transformation. If one bacterium has developed resistance to an antibiotic, it can pass that resistance on to other bacteria. This process can lead to the rapid spread of resistance genes among bacterial populations, turning a once-treatable infection into a persistent, resistant one.
-
Use of Broad-Spectrum Antibiotics: Instead of targeting a specific pathogen, broad-spectrum antibiotics affect a wide range of bacteria, including beneficial ones. This can disrupt the natural balance of microorganisms in the body, allowing antibiotic-resistant bacteria to thrive and dominate, possibly leading to persistent infections.
-
Environmental Persistence: Antibiotics that end up in the environment, whether through agricultural runoff or insufficient wastewater treatment, can expose environmental bacteria to low levels of these drugs. Over time, this can promote resistance in these populations. When these resistant bacteria infect a host, they can lead to persistent infections that are harder to treat.
-
Suboptimal Concentrations: At times, the concentration of the antibiotic reaching the site of infection might be suboptimal due to various pharmacological factors. In such cases, instead of eliminating the bacteria, the antibiotic might only be stressing them, thereby prompting them to develop resistance mechanisms.
Having tangible knowledge and understanding of the way bacteria resist to antibiotics is paramount, as this represents a true public health concern. Persistent and recurrent infections in humans are common, and their frequency is rising. Despite this, our understanding of antimicrobial treatment failure remains insufficient.
- KASPY, I., ROTEM, E., WEISS, N., RONIN, I., BALABAN, N. Q. & GLASER, G. 2013. HipA-mediated antibiotic persistence via phosphorylation of the glutamyl-tRNA-synthetase. Nature Communications, 4. Article number 3001
- ALDRIDGE, B. B., FERNANDEZ-SUAREZ, M., HELLER, D., AMBRAVANESWARAN, V., IRIMIA, D., TONER, M. & FORTUNE, S. M. 2012. Asymmetry and Aging of Mycobacterial Cells Lead to Variable Growth and Antibiotic Susceptibility. Science, 335, 100-104
- SILVA, J. 1996. Mechanisms of antibiotic resistance Current Therapeutic Research, 57, 30-35
- KESTER, J. C. & FORTUNE, S. M. 2013. Persisters and beyond: Mechanisms of phenotypic drug resistance and drug tolerance in bacteria. Critical Reviews in Biochemistry and Molecular Biology, 1-11.
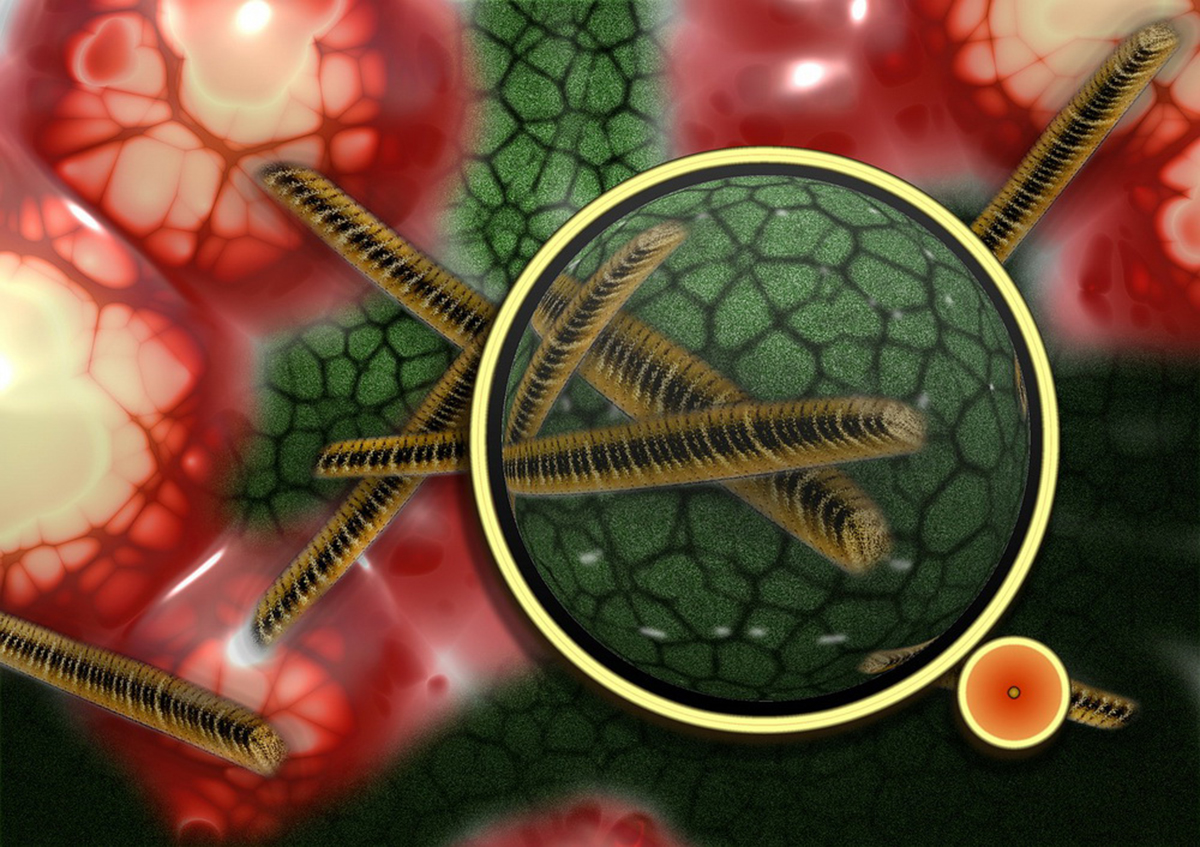
- Photo courtesy of geralt by Pixabay : pixabay.com/en/bacteria-bacterial-species-imitation-108895/
- Photo courtesy of Bmramon by Wikimedia Commons : en.wikipedia.org/wiki/File:NOVAMOXIN_antibiotic.jpg


Your thoughts on this