Table of Contents
More Antibiotic-Resistant Strains of Bacteria Appearing in More Places
At first, MRSA was only a problem in hospitals but nowadays it is found in gyms, nursery schools, and retirement centers. Sometimes healthy people pick up MRSA infections through cuts and scrapes. The dangerous aspect of MRSA is that it has the ability to survive despite exposure to methicillin, the antibiotic given to people with life-threatening infections when other antibiotics fail.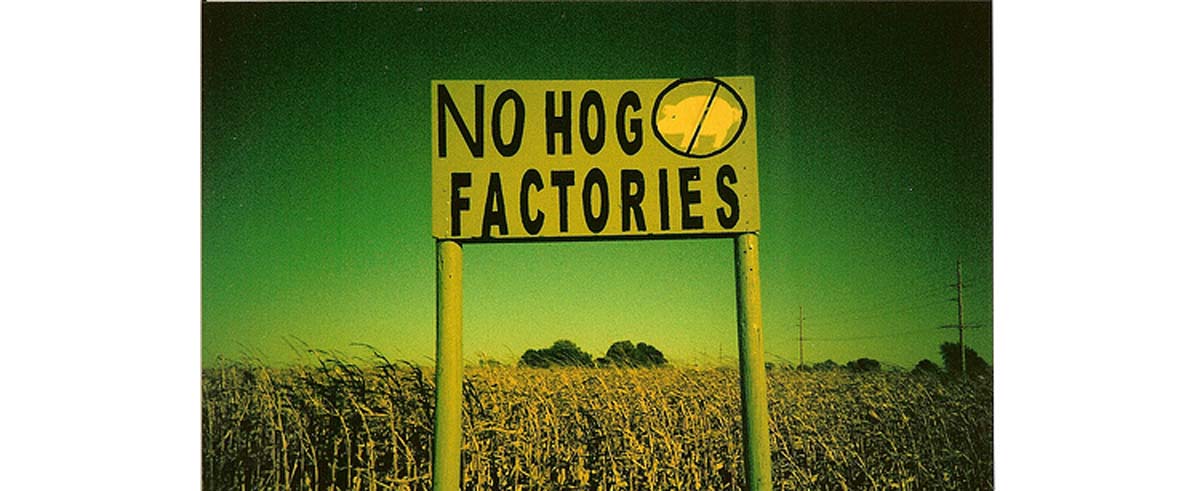
Antibiotic resistance is literally a deadly, serious concern. Even healthy people can become infected with "super bugs" that cannot be treated, death sometimes striking an active, healthy person in just hours. Or even worse, the immune system may resist the infection leading to weeks of agonizing fever, bloating, inflammation, and sepsis before death occurs.
I have to admit a bias on this topic. Both my father and my grandfather died of infections with antibiotic-resistant bacteria, my grandfather of E. coli, and my father of Vancomycin-resistant Enterococcus.
Both had been active, involved senior citizens until they got their infections. Both suffered horribly for months before they eventually died. Describing the actual effects of these infections is still a little too close to me for accurate reporting, but suffice it to say you don't want to get them.
How Bacteria Develop Antibiotic Resistance
Before the 1980's, most antibiotics killed most bacteria. Since the 1980's, doctors are constantly having to introduce new antibiotics to keep infections under control. The way the first bacterium survives an antibiotic treatment is sheer luck. Something causes a mutation in the bacterial DNA.
That mutation leaves one bacterium standing when the treatment is done. If it is destroyed by the immune system, or it is killed by conventional antiseptic treatment, or if it just runs out of food before it divides, that gene does not give any other bacteria the power of antibiotic resistance.
But bacteria can pass genes to others of their species, and even different species, without reproducing. There are several different ways:
- A bacterium can be infected with a virus. The virus latches on to the antibiotic resistance gene and carries it to another bacterium. This process is called transduction.
- A bacterium can rub up against another bacterium and exchange DNA. Although not, strictly speaking, sex, this process allows bacteria to share antibiotic resistance with other microbes. This process is called conjugation.
- And a bacterium can feed on DNA from dead, antibiotic-resistant bacteria, incorporating their genes into its DNA. This process is called transformation. It was first observed in the 1920's by a British biologist named Frederick Griffith. He observed that he could kill a virulent (symptom-causing) strain of Streptococcus pneumoniae and then put the dead, disease-causing bacteria into a live, usually harmless strain of the same bacteria. The usually harmless strain would become a disease-causing strain after coming in contact with dead bacteria.
These processes have been around for millenniums. Why is antibiotic resistance becoming such a major problem now? Some experts believe the culprit is the overuse of antibiotics in livestock feed.
- Tom Levitt, "Overuse of drugs in animal farming linked to growing antibiotic-resistance in humans," The Ecologist, 23 May 2011.
- Photo courtesy of jkgroove on Flickr: www.flickr.com/photos/jkgroove/2218094907/

