Graves’ disease is a disorder affecting multiple organs of the body, caused by hyperactivity of the thyroid gland. The thyroid gland is a small soft gland located at the base of the neck just beneath the larynx and it is responsible for the production of the two main thyroid hormones known as thyroxine and tri-iodothyronine, which are important in the regulation of several metabolic processes in the body.
The main consequence of the elevation in thyroid hormone levels in the uncontrolled increase in metabolism, beyond what is needed by the body.
Graves’ disease occurs about five times more frequently in women as compared to men, and peak incidence is around the 4th to 6th decade of life. It was named after an Irish physician, Robert Graves, who in 1835, first described the constellation of symptoms and signs relating to the disease entity.

What Causes Graves’ Disease?
Graves’ disease is primarily a disorder of the immune system. For reasons which are poorly understood, antibodies, referred to as auto-antibodies, are produced which target the receptors within the thyroid gland, and induce long term stimulation of the gland by interfering with the normal body mechanisms which control thyroid hormone production (Girgis, Champion, & Wall, 2011). These auto-antibodies also result in stimulation of cells in other organs such as the eyeballs and the skin. Inherited genetic defects in the several important pathways in thyroid hormone production have been shown to be important in Graves’ disease (Chu et al., 2011).
What Are The Symptoms Of Grave’s Disease?
- Protrusion of the eyeball, known as exopthalmos, is a major feature of Graves’ disease. It is slow and progressive, and can lead to permanent damage to one or both eyes.
- An enlarged thyroid gland, known as Goitre.
- Rapid, sometimes audible heartbeat, known as palpitations.
- Inability to sleep.
- Sexual dysfunction in men, and cessation of menstrual cycle in women may occur early in the disease.
- Anxiety and emotional irritability.
- Increased perspiration even in a cold environment, worsened by hot weather.
- Increased appetite and a paradoxical loss of weight despite increased dietary intake.
- Constant hand tremors.
- Muscle weakness, more severe in the shoulder and thigh regions.
How Is Graves’ Disease Diagnosed?
Diagnosis of Graves’ disease relies upon the delineation of the characteristic symptoms and signs as well as laboratory investigations. A thorough and extensive clinical examination will be useful not in diagnosis but also to assess disease complications. Laboratory tests on blood samples will be needed to quantify the levels of thyroid hormones and auto-antibodies. Sometimes, a scan of the thyroid gland and/or a biopsy may be necessary to rule out other causes of an enlarged thyroid gland. Other ancillary investigations are important in identifying co-morbidities and narrowing down the best treatment approach.
How Is Graves’ Disease Treated?
The treatment modalities in Graves’ disease depend on several factors.
- Age of patient.
- Severity and complications of the disease.
- Presence of associated co-morbidities.
Antithyroid Drugs
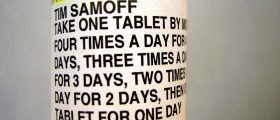
Antithyroid drugs, which exert their pharmacological effect by decreasing the amount of thyroid hormones in the body, are important components of treatment of Graves’ disease. Examples of these drugs include Carbimazole, Methimazole and Propylthiouracil. However, these drugs induce complete disease remission in only about a third of severe cases and about half of mild cases. In routine clinical practice, antithyroid drugs are used to normalize blood level of thyroid hormones prior to radioactive iodine therapy or surgery.
Beta Adrenergic Receptor Blockers
Many symptoms of Graves’ disease such as tremors, palpitations and anxiety can be brought under control by the use of drugs known as Beta-blockers. Examples of these drugs are Propanolol and Atenolol. These drugs do not reduce thyroid hormone levels, but can provide significant symptomatic relief.
Radioactive Iodine
This is the most commonly used form of treatment for Graves’ disease. By using a small amount of radioactive iodine, the excessive thyroid hormone-producing tissue is ablated and the result is hypothyroidism. Following this, patients will require lifelong therapy with thyroid hormones. Treatment usually lasts for about two to four months, during which close monitoring of thyroid hormones is performed. Repeated bouts of treatment may be needed for patients whose serum thyroid hormone levels remain high. When patients become hypothyroid, symptoms of hypothyroidism may occur, such as weight gain. This may require closer monitoring of thyroid replacement therapy.
Close contacts of people on radioiodine therapy, especially children and pregnant women are at risk of exposure to small amounts of radiation. Therefore, close physical contact should be avoided. Radio-iodine is never given to pregnant women due to the risk of congenital malformations. Furthermore, treatment of Graves’ disease in pregnancy requires careful consideration of maternal and foetal thyroid functions and possible complications(Laurberg, Bournaud, Karmisholt, & Orgiazzi, 2009).
Surgical Treatment Of Graves’ Disease
This is the least preferred option due to the risks of damage to many delicate tissues such as nerves and the parathyroid gland.
However, there are situations in which surgical treatment is recommended.
- In cases of airway obstruction by large goitres.
- Suspected cases of cancerous growths within enlarged thyroid gland.
- When both anti-thyroid drugs and radioiodine are contra-indicated.
- Chu, X., Pan, C. M., Zhao, S. X., Liang, J., Gao, G. Q., Zhang, X. M., . . . Song, H. D. (2011). A genome-wide association study identifies two new risk loci for Graves' disease. Nat Genet, 43(9), 897-901. doi: 10.1038/ng.898
- Girgis, C. M., Champion, B. L., & Wall, J. R. (2011). Current Concepts in Graves' Disease. Therapeutic Advances in Endocrinology and Metabolism, 2(3), 135-144. doi: 10.1177/2042018811408488
- Laurberg, P., Bournaud, C., Karmisholt, J., & Orgiazzi, J. (2009). Management of Graves' hyperthyroidism in pregnancy: focus on both maternal and foetal thyroid function, and caution against surgical thyroidectomy in pregnancy. Eur J Endocrinol, 160(1), 1-8. doi: 10.1530/eje-08-0663
- Photo courtesy of SteadyHealth












-In-Infants-And-Older-Children_f_280x120.jpg)

