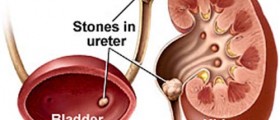
Ureter stents are common and 74 percent of patients with some form of urinary stones will require this device to be used. Stones are a problem in 11 percent of men and 7 percent of women so don't worry, you are definitely not alone in your grief and uncertainty.
When it is ultimately time to remove these stents, there are two acceptable practices that patients can use to remove the device successfully. Patients lacking confidence in their abilities to remove it themselves or who may not be physically able to can visit their urologist or nephrologist depending on the country you are living in and he will be able to remove it with a simple office cystoscopy. This is the case of what happens 44 percent of the time. Should you be more confident in your abilities, stents are able to be removed by strings attached to the device. This can be done in 39 percent of cases.
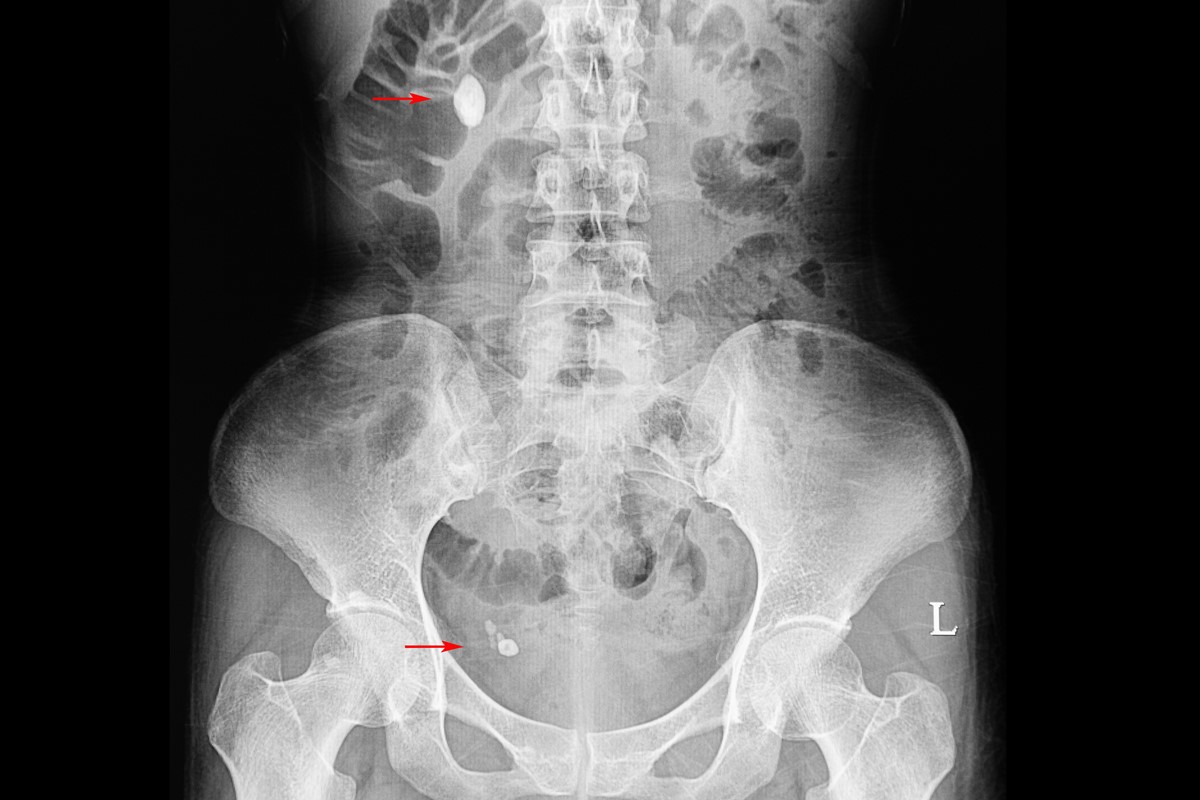
When considering what option is right for you, the most prevalent morbidity that patients will face is moderate-to-severe pain that will accompany the device being removed. In a study of 571 patients who had to remove their stents, patients reported on average a pain level of 5 out of 10 subjectively. Patients also reported that when visiting a physician, the pain levels were slightly higher than what you would experience if you removed the device by a string. After the initial insult of pain, 32 percent of patients reported delayed severe pain after the stent was removed and even 10 percent needed to visit their local emergency rooms to deal with unexpected complications. [1]
I will focus on the string removal method primarily in this response because this would be the self-removal option that this chat group is focusing on. String removal is generally considered when patients are given a double J ureter stent. This may not mean anything to you medically but this is the "gold-standard" therapy to promote the flow of urine after a placement of the stent. These stents are based on a patient's height and strings are usually left hanging from the ureter meatus with no need to attach it to your skin with sutures.
Once this stent is in place, patients will be discharged with some type of prophylactic antibiotic to avoid infections and a pain-killer generally in the form of a non-steroidal anti-inflammatory drug (NSAID) for the first week. In most cases, stents can be removed by the 7th-day post-operation.
When stents are removed by string, it is nearly impossible for medical professions to apply lidocaine to the wall of the ureter because of the possibility of inadvertently tearing the string. Should you choose an option without a string, lidocaine can be applied, however.
In one study, 114 patients were grouped based on string vs. no string groups. Although both groups reported similar levels of pain, general health, and urinary symptoms while the device was in place, there was a significantly higher portion of patients with strings attached to their stents that experienced dysuria and problems with sexual activity.
At the conclusion of the study, interestingly enough, even if with the symptoms linked with strings attached to stents, 16 of 20 patients reported that they would rather have their stents removed by string again compared to previous methods they endured in the past. [2]
Due to the complications that can be potentially linked with removing a stent from a string, I encourage all those who are considering self-removal to make an appointment instead with your local urologist. String-breaking or after-bleeds are rare but can cause serious complications so it is best to use the skilled hand of a medical professional to make sure that these risks are less likely to happen.
- Photo courtesy of SteadyHealth