This can be caused directly by some drug, toxin, blood parasite virus or some other known cause, or it can be an unexplained immune mediated reaction.
Incidence
Hemolytic anemia represents approximately 5% of all anemias. The overall incidence of death is caused by this disorder is low. However, older patients and patients with cardiovascular impairment are at an increased risk. Most of the disorders that lead to hemolysis are not specific to any race or gender.
Signs and symptoms of autoimmune hemolytic anemia
Since there is often some kind of underlying disorder behind this type of anemia, symptoms are usually caused by both anaemia and the underlying disorder. It is also important to know that patients with minimal haemolytic anaemia can be asymptomatic.
Severe anaemia, especially of sudden onset, may cause:
- tachycardia,
- dyspnoea,
- angina
- weakness
- tiredness
- faintness
- dizziness
- general pallor and pale conjunctivae
- tachycardia
- tachypnoea – fast breathing
- hypotension
- mild jaundice may occur due to haemolysis.
- dark urine
When destruction persists for a few months or longer, the spleen may enlarge, resulting in a sense of abdominal fullness and discomfort.
Possible causes of hemolytic anemia
Genetic
This condition can be caused by some red cell membrane abnormalities such as hereditary spherocytosis or elliptocytosis.
It can also be caused by some hemoglobin abnormalities such as sickle cell anaemia or thalassaemia. Some enzyme defects such as Glucose-6-phosphate dehydrogenase and pyruvate kinase deficiency can also be the underlying disorder.
Immune
Isoimmune:
- haemolytic disease of newborn
- blood transfusion reaction
Autoimmune:
- Warm antibody type: idiopathic, SLE, lymphoma, chronic lymphatic leukemia, Evans' syndrome.
- Cold antibody type: cold haemagglutinin disease, paroxysmal cold haemoglobinuria, mycoplasma pneumonia, lymphoma, infectious mononucleosis or other viral infections, chronic lymphatic leukemia.
- Drug related: drug absorbed onto red cell surface, e.g. penicillin, cephalosporins, or immune complex mediated, e.g. sulphonamides, quinidine.
Other causes:
- Non-immune
- trauma,
- cardiac haemolysis,
- micro-angiopathic anaemia
- haemolytic uraemic syndrome
- thrombotic thrombocytopenic purpura
- infection
- hypersplenism - enlarged lien
- membrane disorders,
- paroxysmal nocturnal haemoglobinuria,
- liver diseases
Excessive blood loss may also occur over a long period of time (chronic bleeding):
- Heavy menstruation
- Bleeding cancer or polyps in the gut
- Bleeding gastric or duodenal ulcers
- Nosebleeds
- Bleeding hemorrhoids
Mechanism and course of the disease
Hemolytic anemia occurs when the bone marrow is unable to compensate premature destruction of red blood cells by increasing their production. Red blood cells are being destroyed by autoantibodies. This may occur suddenly, or it may develop gradually. In some people, the destruction may stop after a period of time while in other people, it persists and becomes chronic. What triggers these antibodies to attack these red blood cells is still unknown. Haemolysis may occur by two mechanisms:
Intravascular
This type occurs most commonly due to complement fixation, trauma, or other extrinsic factors. The most common triggers are:
- prosthetic cardiac valves,
- glucose-6-phosphate dehydrogenase deficiency,
- thrombotic thrombocytopenic purpura,
- disseminated intravascular coagulation
- paroxysmal nocturnal haemoglobinuria
- Extravascular
The red blood cells are removed from the circulation by the mononuclear-phagocytic system either because they are defective or there is the presence of bound immunoglobulins on their surfaces.
The etiology of premature erythrocyte destruction is diverse and can be caused by conditions such as:
- intrinsic membrane defects,
- abnormal hemoglobins,
- erythrocyte enzymatic defects,
- immune destruction of erythrocytes,
- mechanical injury,
- hypersplenism
Types of hemolytic anemia
There are two main types of autoimmune hemolytic anemia:
- Warm antibody hemolytic anemia – the autoantibodies attach to and destroy red blood cells at temperatures equal to normal body temperature
- Cold antibody hemolytic anemia - the autoantibodies become most active and attack red blood cells only at temperatures well below normal body temperature
Diagnosis of hemolytic anemia
Anaemia can be easily identified by simple blood tests measuring the number of red blood cells and the amount of hemoglobin in the blood.
Blood tests
- CBC count
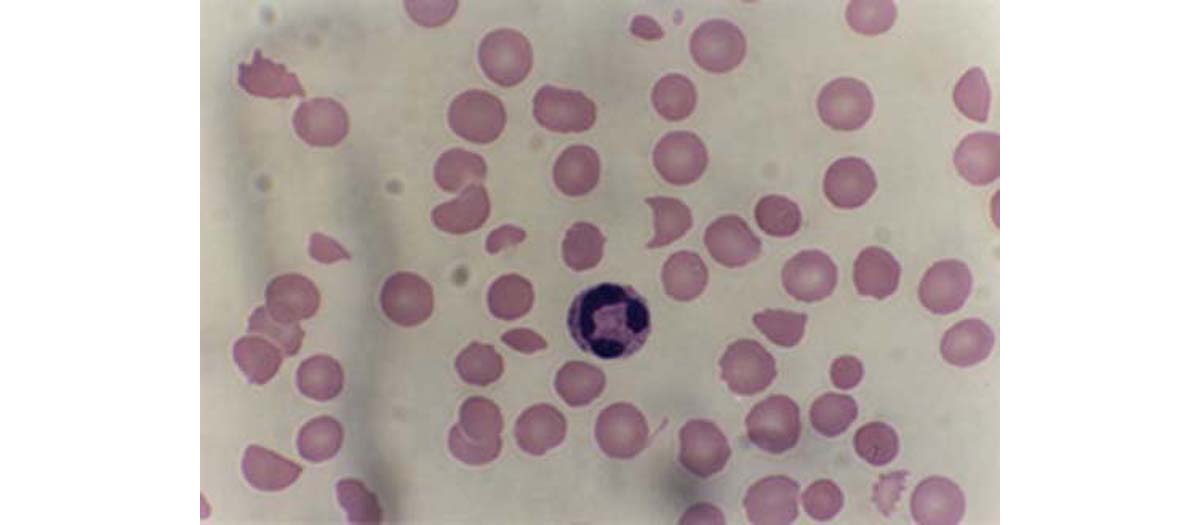
- Peripheral smear and morphological examination
- RBC indices
- Increased red blood cell distribution width (RDW) study
- Reticulocyte count
- Lactic acid dehydrogenase test
- Serum haptoglobin
- Indirect bilirubin
- Potassium test
- Platelet count
- Peripheral smear
- Leukocyte alkaline phosphatase
- Serum iron
- Hematocrit
- Ferritin
Results of the blood studies should show the
following:
- Elevated indirect bilirubin levels
- Low serum haptoglobin
- Hemoglobin in the urine
- Hemosiderin in the urine
- Increased urine and fecal urobilinogen
- Elevated absolute reticulocyte count
- Low red blood cell count (RBC) and hemoglobin
- Elevated serum LDH
Imaging studies
The ultrasound may be used to estimate spleen size. The physical examination occasionally does not detect significant splenomegaly. Chest radiograph is used to evaluate cardiopulmonary status.
There is a specific procedure to diagnose an autoimmune type of anemia. Autoimmune haemolytic anaemia is diagnosed by the presence of antibodies that bind to red cells in the blood.
Treatment of autoimmune hemolytic anemia
The good thing is that, if symptoms are mild or if destruction of red blood cells seems to be slowing on its own, no treatment will be needed.
Corticosteroids
If red blood cell destruction is worsening, some corticosteroid drugs such as Prednisone are usually the first choice for treatment. They should suppress the immune system which is usually overactive. High doses should be used at first and then a gradual decreasing of the dose should follow over many weeks or months.
Surgical solutions
When people do not respond to corticosteroids, a surgery to remove the spleen is often the next choice of treatment. This operation is called splenectomy. Splenectomy is not recommended in hemolytic disorders such as cold agglutinin hemolytic anaemia.
Immunosuppressive drugs
When destruction of red blood cells persists after removal of the spleen or when surgery cannot be performed, immunosuppressive drugs, such as Cyclophosphamide or Azathioprine, are used to suppress the immune system response.
Plasmapheresis
Plasmapheresis is a specific procedure which involves filtering blood to remove antibodies. It is occasionally very helpful when other treatments fail.
Transfusion therapy
When red blood cell destruction is severe, blood transfusions are needed. The problem is that they do not treat the cause of the anemia and provide only temporary relief. In these disorders, type matching and cross-matching may be very difficult. The risk of acute hemolysis of transfused blood is high, but the degree is dependent on the rate of infusion.
Iron therapy
Studies have shown that this is indicated for patients with severe intravascular hemolysis in which persistent haemoglobinuria has caused substantial iron loss.
However, since iron stores increase in hemolysis, iron administration is generally contraindicated in hemolytic disorders.
Possible complications
- Anaemia: high output cardiac failure.
- Jaundice: increased unconjugated bilirubin.
- In intravascular hemolysis, iron deficiency due to chronic haemoglobinuria can exacerbate anaemia and weakness.
Tips for people with this disorder
Diet tips
Fava beans can cause severe hemolysis in certain patients with this disorder and thus eating dishes with fava beans shoud be avoided.
Medications
Medications and chemicals that should be avoided are:
- Acetanilide
- Furazolidone
- Isobutyl nitrite
- Nalidixic acid
- Naphthalene
- Niridazole
- www.nlm.nih.gov
- www.hcd2.bupa.co.uk
- en.wikipedia.org/wiki/Autoimmune_haemolytic_anaemia

