Up to 40 percent of fibromyalgia patients additionally battle ankylosing spondylitis. Living with this combination of diagnoses worsens the symptoms of both, including pain, inflammation, and poor sleep — and their complications, or other health issues you're burdened with, can really send you into symptom overload.
What do ankylosing spondylitis and fibromyalgia have in common, and what are the differences?
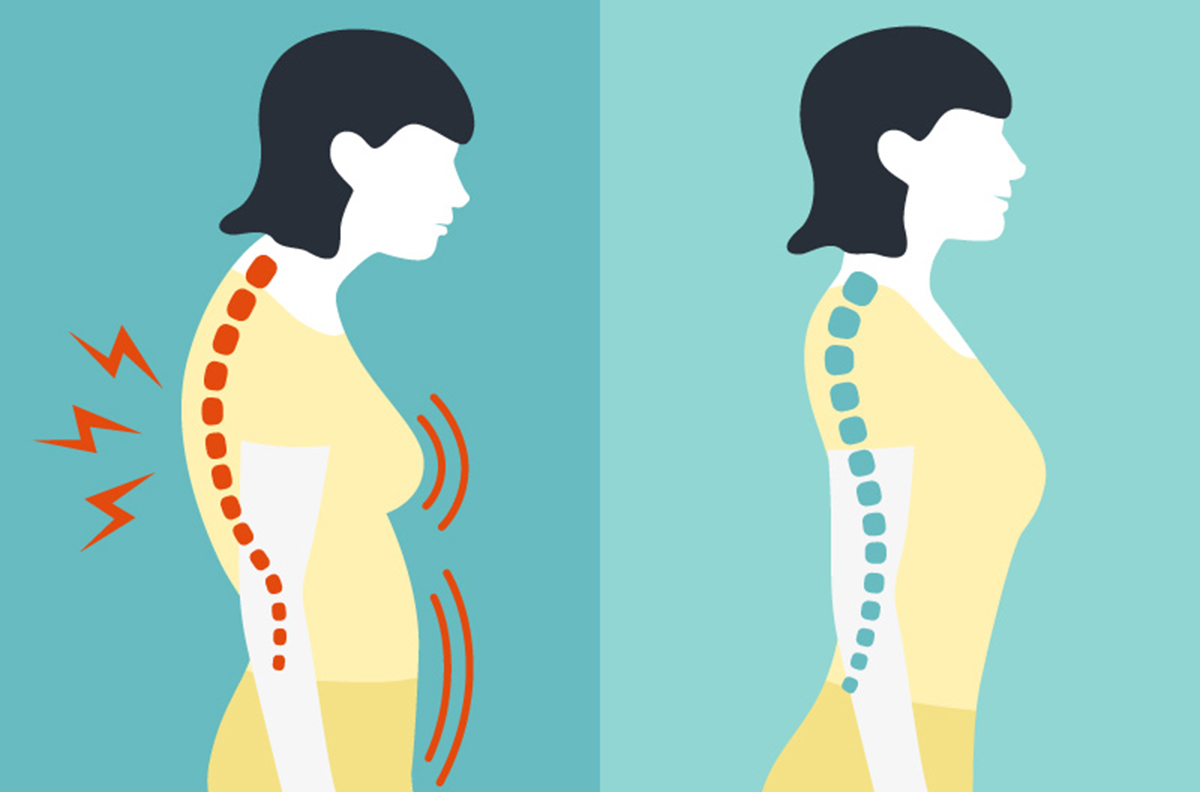
Ankylosing spondylitis will, as a form of arthritis that mostly strikes the spine, induce pain and stiffness across the back, from your neck to your backbone. The inflammation resulting from the condition can lead to chronic pain that worsens over time, and in some cases, your vertebrae may even fuse, severely restricting your mobility. Though ankylosing spondylitis is known as a spinal condition, other parts of the body, like the shoulders, hips, ribs, and even your hands and feet may also be affected.
Fibromyalgia is, on the other hand, a functional pain disorder with an as yet unknown cause. Its main symptoms are widespread pain, so-called tender points, fatigue and sleep disturbances, and cognitive problems such as mood swings and short-term memory loss. Though pain is the most universal symptom, fibromyalgia doesn't appear to cause inflammation. The current theory is that fibromyalgia changes the way in which your brain reacts to pain stimuli, thereby making patients hypersensitive — even to touch that isn't normally painful at all.
Pain and poor sleep quality — which interact with each other in obvious ways, as pain makes it hard to sleep and fatigue can worsen pain — are the obvious connections between ankylosing spondylitis and fibromyalgia. Any chronic pain condition that robs you of the sleep quality you deserve places you at a higher risk of also developing fibromyalgia. Until genetic research can find common genetic markers between the two conditions, any further link will remain unclear.
How is ankylosing spondylitis diagnosed?
Ankylosing spondylitis is diagnosed by a rheumatologist, on the basis of:
- A physical examination and a discussion about the symptoms you are experiencing
- A discussion about your own medical history and that of your close relatives
- X-rays
- Blood tests
- Measuring your check as you breathe
- Results of lab tests
Ankylosing spondylitis: Your treatment options
Helping you find relief from your symptoms — primarily pain and stiffness — will be your physician's number-one priority when deciding what treatment will work best for you. Treatment additionally serves to prevent longer-term complications of ankylosing spondylitis. This means that you'll be working on your posture with maintaining normal function and mobility in mind. As such, you won't be surprised that a combination of lifestyle changes and medication are almost certain to make up your treatment plan:
- Physical and occupational therapy helps you stay mobile and functional, and reduces the risk of permanent disability. The earlier you start, the more effective this therapy is likely to be.
- Exercise plays an incredibly important role in reducing your stiffness. It will also lead to stronger muscles, and thereby help maintain functionality. Swimming is an example of a form of exercise that is safe and extremely beneficial for people with ankylosing spondylitis.
- Deep breathing exercises have the dual purpose of acting as stress-relief and keeping your chest flexible — since the ribs are sometimes affected, this is especially important.
Pharmacological treatment will likely include:
- Some form of nonsteroidal anti-inflammatory (NSAID). These include ibuprofen, naproxen (Aleve), and Aspirin, and they fight inflammation and pain at the same time. Though they are available over the counter, be sure to discuss the appropriate dosage with your rheumatologist.
- Disease-modifying antirheumatic drugs (DMARDs) include methotrexate (Rheumatrex), but also biologic agents like adalimumab (Humira) and adalimumab-atto (Amjevita).
- Steroid injections aren't on the cards as a regular, recurring treatment, but they can help greatly in some cases.
- Antidepressants may likewise play a role in your treatment, even if you are not depressed — some, including Cymbalta, have been shown to be quite effective in the fight against chronic back pain.
- Finally, surgery to improve your posture or replace a joint is an option in some cases.
Lifestyle changes that can help with ankylosing spondylitis
Making changes to the way you sleep leads to a big improvement for some people, so wherever possible, try:
- To buy a firm, supportive mattress if you do not already have one
- Sleeping with a straight spine — this is why propping your upper body up with pillows, an instinctive reaction to the pain for some people, isn't recommended
- Asking your physical therapist to recommend improvements you can make to your work space, or to suggest a specific chair and desk that support a good posture
In addition, don't use tobacco, which can worsen both your symptoms and your condition, and be extra weary of falls, jumps, and sudden movements because your back and neck are more prone to injury than they are in the average person.
Fibromyalgia: Treatment options
Looking at the medications typically used to treat fibromyalgia, you'll see some "familiar faces" — pain relievers and antidepressants are also often used to manage ankylosing spondylitis.
Over-the-counter pain relievers recommended for fibromyalgia patients will include acetaminophen as well as the same NSAIDs that benefit people with ankylosing spondylitis, which still relieve pain even if they don't need to fight inflammation in people who only have fibromyalgia. Tramadol, a prescription opioid also sold under the brand name Ultram, is also sometimes used in fibromyalgia treatment. Beware that narcotics can lead to tolerance and even addiction over time quite easily.
Antidepressants fibromyalgia patients will often find themselves being prescribed include Duloxetine (Cymbalta) and milnacipran (Savella). These are not just for depression, but also help fight pain and fatigue.
Another option that promotes a better sleep quality is amitriptyline, often used for depression and anxiety. Cyclobenzaprine is a muscle relaxant, and it may also enable people with fibromyalgia to achieve the sleep they need.
Anti-epilepsy drugs were designed to reduce the frequency of seizures, but have been found to be useful for many other purposes as well. In fibromyalgia patients, Gabapentin (Neurontin) and Pregabalin (Lyrica) have proven especially helpful when dealing with pain. Pregabalin was specifically FDA-approved for this purpose.
As with ankylosing spondylitis, lifestyle changes and other non-pharmacological treatments can be just as important as medications. Treatments that may help you include:
- Occupational therapy, specifically learning to carry your daily responsibilities out in a way that supports, rather than hurts, your body, and learning to create work and living spaces that preserve your health and posture.
- Physical therapy involves a kind of exercise, under the watchful eye of a physical therapist. It serves to increase your strength and flexibility, promote fitness, and improve your posture.
- Talk therapy, cognitive behavioral therapy for example, can't just help you work through the stress you face as the result of your chronic medical conditions, but also teach you breathing and other techniques to help you through particularly painful periods.
In conclusion
People with ankylosing spondylitis will need to be under the care of a rheumatologist, but the very same doctor will also most likely be able to work with you to map out a treatment plan for your "fibro". Other doctors you may see over the course of your "patient career" include internists, physical therapists, psychotherapists (either a psychologist or a psychiatrist), pain specialists, and of course also your primary care doctor. Together, your medical team will work on reducing your pain, and increasing your sleep quality, energy levels, and physical strength.
- Photo courtesy of SteadyHealth.com

