When Americans check the box on their driver's license renewals that volunteers them to become a donor for transplants, most probably aren't thinking they could contribute to fecal matter transport, also known, to use one of the politer terms, as a poop transplant.
Fecal matter transplants aren't harvested from cadavers. They're taken from healthy people. In fact, there are people who earn a substantial supplemental income for feces donation.

Why Would Doctors Think It's a Good Idea to Transplant Poop?
One of the most prominent features of fecal matter that you probably weren't ever told in a biology class is that about one-third of the mass of stool is living bacteria. The bacteria in our solid waste are the bacteria that live in our guts. There are up to 2,000 species of bacteria numbering about 10 trillion individual bacteria in the typical human adult colon. At any given time, you are probably carrying around 1000 to 1500 grams (2 to 3 pounds) of bacteria. Some of these bacteria are beneficial. They break down fibers, or they produce useful fatty acids and vitamins, or they protect against bacterial infections through sheer numbers; they don't give pathogenic bacteria a chance to accumulate in the bowel. Some of these bacteria are harmful if they grow to excessive numbers. Sometimes antibiotic treatment for an infection with one kind of bacteria can cause a "bloom" of another, disease-causing kind of bacteria. That's the problem with an infection called Clostridium difficile (or C. difficile).
Clostridium bacteria are everywhere. They're in the ground. They're in our food. They are in our bowels. Most of the time they don't cause any real problems unless they grow to excessive numbers. Then they can cause chronic symptoms such as watery diarrhea, abdominal pain more or less all the time, loss of appetite, severe fatigue, and fever. Those symptoms will make you sick, but treating Clostridium difficile infections, ironically, sometimes kills the bacteria that keep Clostridium from becoming even more abundant. A significant percentage of people who get this infection either have to have part of their colon removed, or develop a system condition called sepsis, and about 3 percent of the half-million Americans who get the infection every year die. Even if death doesn't retuls, once you have had a relapse of the infection, it becomes very hard to treat.
READ Fecal Incontinence: Causes, Diagnosis, Treatment
Since the antibiotics (vancomycin and metronidazole in particular) used to treat C. difficile can also cause C. difficile, doctors sometimes treat the infection by restoring fecal bacteria directly to the colon with a transplant. Introduced to the colon through a nasogastric tube, a colonoscopy, or an enema, hundreds or even a couple thousand kinds of helpful bacteria reintroduced to the colon can keep the infection in check. While about two-thirds of people who have one relapse will have another, and maybe another, about 95 percent of people who receive fecal matter from a donor are cured.
Fecal Matter Transplants Aren't Just for C. difficile Infections
Some other hard-to-treat bowel problems can benefit from fecal matter transplantation, notably some cases of irritable bowel syndrome (IBS). There are even reports of dramatic improvement in obesity, type 1 diabetes, type 2 diabetes, rheumatoid arthritis, Sjogren's disease, and Parkinson's disease after fecal matter transplant. Whether this procedure will work for you is something you need to work out with your doctor, but here is an outline of how it works.
What's the Procedure for Fecal Matter Transplantation?
The first step in fecal matter transplantation is finding a donor. While there's no such thing as a perfect poo donor, not just anyone qualifies as source of healing poop. Obviously, you don't want someone who has communicable diseases like HIV, syphilis, or hepatitis A, B, C, or E. You also don't want anyone who has antibiotic treatment of any kind in the last six months. Any history of intravenous drug use, risky sex, or incarceration is usually disqualifying, as are recent travel to regions that have endemic diseases and tattooing or body piercings that are less than six months old.
Not just the donor but also the feces itself have to be of suitable quality. An August 27, 2015 CNN story reports these guidelines from the Open Biome Project in Boston:
"Types one or two, defined by the Bristol Stool Chart as 'like nuts; or 'lumpy,' are too dry to process into a treatment.
If a donor’s stool is 'mushy' or 'watery' — that’s a type six or seven — then it can’t be used because it could be a sign the donor has a gastrointestinal infection.
The perfect poop is type three, which is 'like a sausage but with cracks on its surface;' type four, which is 'like a sausage or snake, smooth and soft;' or type five, 'soft blobs with clear-cut edges (passed easily).'"
Even when doctors are working with a known donor, they test each sample for the presence of parasites, to make sure they are not passed on to the recipient.
When doctors find a highly desirable donor with reliably highly desirable poop for fecal transplants, they tend to keep asking for more. Feces donors are paid for their contributions. Some people earn $1000 to $1100 a month for donating feces for transplant. Many donors take their part time job very seriously, and become careful to eat wholesome, natural, organic foods to produce wholesome, natural, organic, well, feces for people who are sick.
Although researchers are working on "poop pills" that can be taken like any other medication, most of the time the donation is given to the patient by colonoscopy or enema. When the small intestine is also involved, the feces may be sent to the bowel through a tube that goes through the nose and down the throat and stomach.
Receiving a fecal matter transplant is unpleasant, but not difficult. You have to stop antibiotics at least a couple of days before the procedure. You need to prepare the same way you prepare for a colonoscopy, by consuming a liquid diet and taking large volumes of laxatives to clean out your colon. The procedure itself takes no more than about an hour, and chances are that you will be given a sedative like Versed so you don't remember it.
READ The New Weapon Against Infection: Fecal Transplant Pills
Even when fecal transplants are given to people in the end stage of C. difficile infection, they are about 70 percent infection. For patients who are not at the point of death, they are about 95 percent effective. Just remember that this is not something you can do at home. (Some have tried.) Unless you happen to be both a doctor and a microbiologist, you can't choose the right donor and the right donation to correct your health problem. When you need a fecal matter transplant, leave it to the professionals.
- Laidman J. Fecal transfer proves potent clostridium difficile treatment. [serial online]. Medscape Medical News. http://www.medscape.com/viewarticle/777772.
- van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013 Jan 31. 368(5):407-15.
- Photo courtesy of scragz: www.flickr.com/photos/scragz/7491575442/
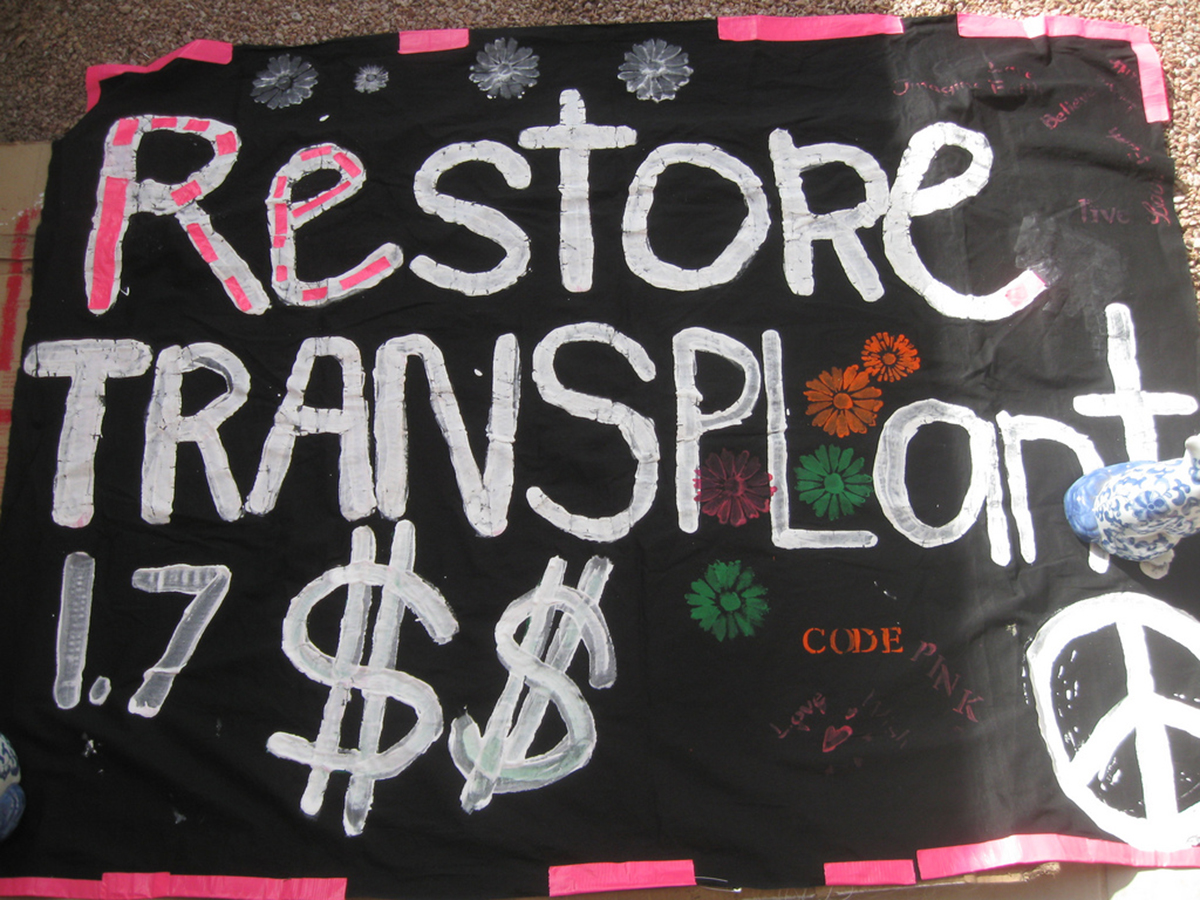
- Photo courtesy of codepinkarizona: www.flickr.com/photos/codepinkarizona/5509919293/
- Photo courtesy of scragz: www.flickr.com/photos/scragz/7491575442/


Your thoughts on this