Table of Contents
Medical terminology can be complex. Understanding your options regarding medical treatment is essential when writing your advanced directive. A misunderstanding about what certain medical care means may prevent you from choosing what is right for you.
What Is Code Status?
One of the most common healthcare instructions in an advanced directive is code status. Code status refers to whether you want certain interventions implemented in a life-threatening situation, such as if you had a cardiac arrest. Further explanation of code status includes:
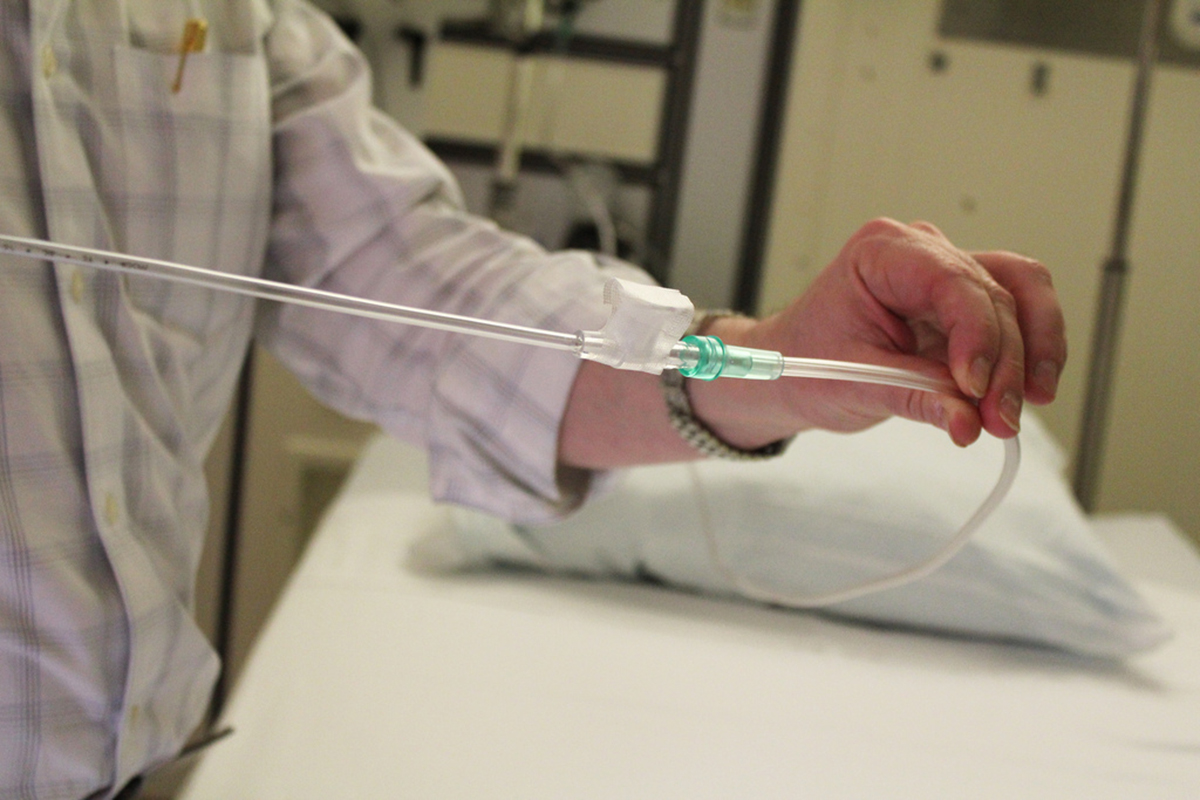
Full Code: A full code involves all measures necessarily to try to save a person’s life. It includes procedures, such as CPR, administration of medication, and defibrillation. In may also involve insertion of a breathing tube to assist with ventilation and the assistance of a mechanical ventilator.
Limited Code: People who are a limited code only agree to some resuscitation procedures. A limited code can mean different things to different people. If you choose a limited code status, you need to state which procedures you want. For example, you may agree to medication and CPR, but not want to be placed on a mechanical ventilator.
Do Not Resuscitate: If you do not want any lifesaving interventions, such as CPR, mechanical ventilation or medications, your instructions should include a do not resuscitate code status (DNR). Keep in mind, making yourself a DNR does not mean you will not receive treatment. Pain medication and other treatment will still be provided.
Advanced Directives Considerations
Before you write an advanced directive, there are several things to take into consideration. For starters, if there is something you don’t understand about medical treatment or care, ask your physician.
Whether you want to change code status, healthcare instructions or your power of attorney, you have the right to do so whenever you wish.
It is also a good idea to discuss your advanced directive with family members. Family members may sometimes have different ideas on what is appropriate for their loved one. For example, it can be difficult to accept a loved one does not want lifesaving measures implemented if their heart stops. Letting your loved ones know about your advanced directive keeps everyone on the same page.
When it comes to the legal aspects of the directive, there is not one specific form, which must be used. You can seek the assistance of a lawyer or write it yourself. There are also many organizations, which can help you draw up an advanced directive if you are unsure of how to do it.
See Also: How to survive a heart attack when you are all alone?
Keep in mind, writing an advanced directive is a very personal decision, which you need to give a lot of thought. Lots of factors go into an advanced direction. Your health, age and personal beliefs all play a part in deciding what is best for you. Even if family members do not agree with your decisions, never allow yourself to be pressured regarding any aspect of your advanced directive.
- www.mayoclinic.org/healthy-living/consumer-health/in-depth/living-wills/art-20046303
- http://www.oag.state.md.us/Healthpol/infosheet.pdfPhoto courtesy of Taberandrew by Flickr: www.flickr.com/photos/andrewbain/521898569
- Photo courtesy of KOMUnews by Flickr: www.flickr.com/photos/komunews/6336510146
- Photo courtesy of Quinn.anya by Flickr: www.flickr.com/photos/quinnanya/5645545829

