Table of Contents
It is clear that an obvious common link between the two diseases does not exist, yet there is enough scientific evidence to suggest that there is a link between the two diseases. In fact, the risk of developing periodontal disease is almost 2.5 times more when compared to a non diabetic individual.
The answer to this may lie in Advanced Glycation End products (AGEs) which are formed during Diabetes. These products get accumulated in different tissues of the body and cannot be removed. They then cause an inflammatory reaction, leading to the activation of the host defense mechanisms of the body against its own tissues, eventually causing destruction and damage.
This is the same pathology that affects other organs all over the body. The presence of these AGEs in the connective tissue of the periodontal tissues has been confirmed thanks to histologic studies.
If the entire surface area of the periodontal ligament is added up around each tooth, then it is roughly the size of an average fist. This is a large enough area to affect the systemic health of person if it is inflamed and infected.
Periodontal disease is an inflammatory disease that releases the products of inflammation like cytokines and prostaglandins all over the body. These mediators of inflammation go and interact with the receptors responsible for transport of essential nutrients across the cells. The end result is a decrease in the sensitivity of these receptors to insulin which leads to a hyperglycemic state in the body also known as Diabetes.
This theoretical relationship between the two diseases can only be proven if there are real-world benefits of treating the one or the other as well in a decrease in complications in well maintained patients.
Can Treatment Of One Affect The Other?
The evidence is very strong regarding the affect diabetes has on periodontal disease, while it is weaker and requires more clinical studies when it comes to the other way round. Every parameter from incidence of disease to severity of disease, and treatment success as well as long-term stability was found to be improved as the glycemic control of the patient improved. This is extremely significant and has huge ramifications for treatment planning.
Similarly, glucose levels were found to be better managed in patients after they had undergone periodontal therapy to help control the disease. As mentioned earlier, this link – while theoretically sound – is more difficult to prove in practice due to the huge number of things that can affect diabetes.
See Also: Complications Of Diabetes: Not So Sweet
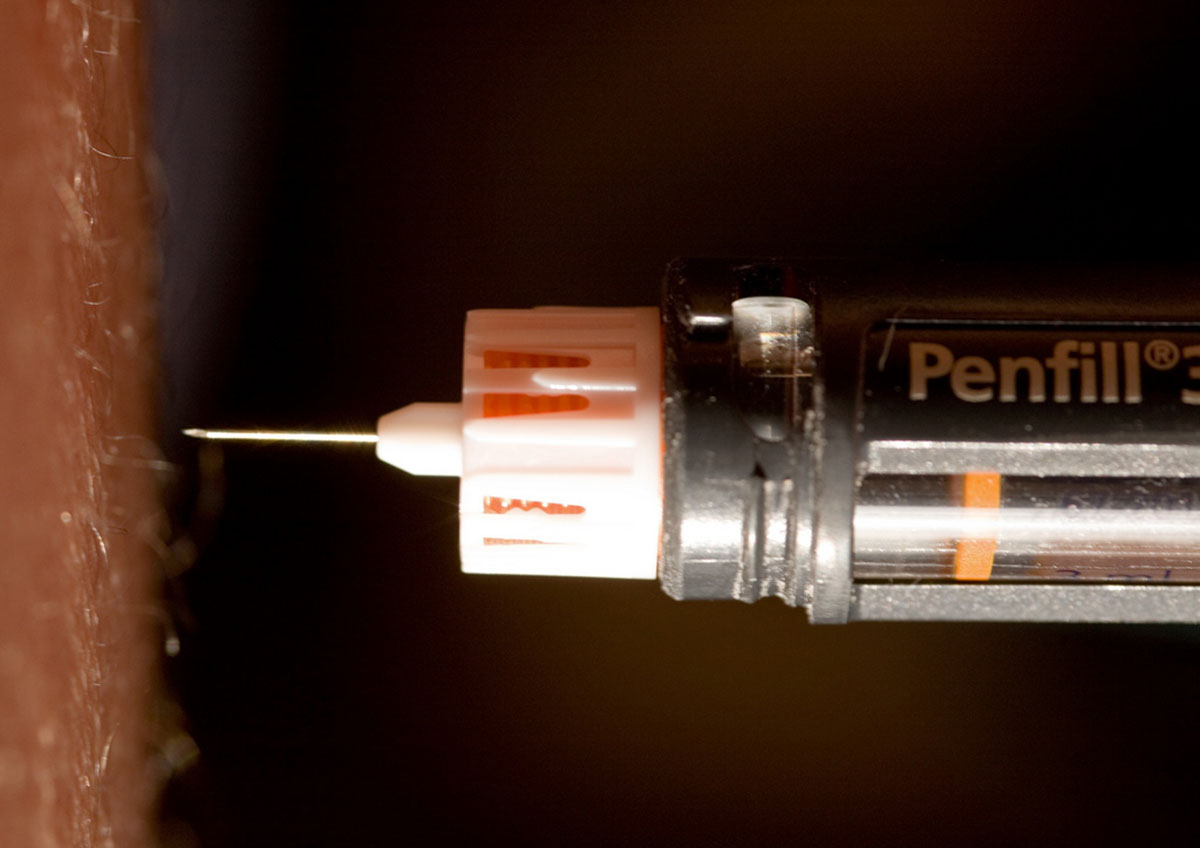
- Photo courtesy of eMuse Tess Heder
- Photo courtesy of Aldenchadwick via Flickr: www.flickr.com/photos/aldenchadwick/2235945601
- 1. Diabetologia. 2012 Jan
- 55(1): 21–31.Published online 2011 Nov 6. Periodontitis and diabetes: a two-way relationship
- 2. http://www.webmd.com/diabetes/periodontal-disease

