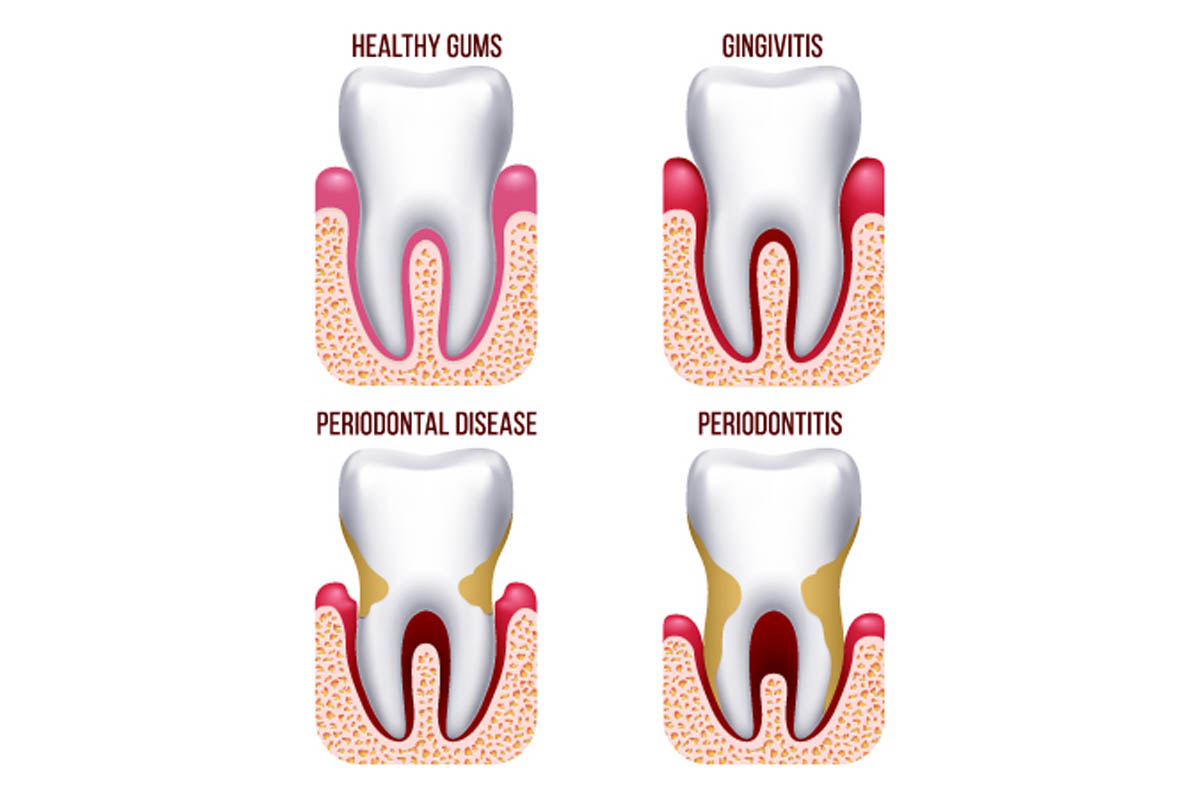
Periodontal diseases generally result from infection or inflammation of the gums and other surrounding supportive structures, including bone. Early on, in gingivitis, the gums may swell and appear red and have a tendency to bleed. When the disease advances to periodontitis, the gums can retract from the teeth, the bone may be damaged, and teeth may become loose or fall out. The periodontal disease generally affects adults and, alongside decay is one of the key threats to dental health.
Reports suggest the following facts about periodontitis:
-
Nearly half of adults aged 30 years plus have periodontal disease in some form.
-
Periodontal Disease becomes more likely with age-approximately seven out of ten, adults 65 years and older have the condition.
-
It is more common in men than women, those living in poverty, those with less than a high school education, and current heavy smokers.
Gingivitis
Gingivitis is a term used to describe inflammation of the gums (gingiva) which arises bacteria remains on the teeth and forms plaque, which in turn can form to become tartar. Gingivitis is not destructive, unlike more severe forms, but if not treated it can advance to periodontitis which in severe cases can result in the loss of teeth.
The gingival disease is seen in two main forms:
-
Dental plaque-induced gingival disease: This may result from the presence of plaque, systemic factors, as a side-effect from medicines, or poor diet (to the extent of malnourishment).
-
Non-plaque induced gingival lesions: This might arise from a specific bacterium, virus, or fungus or be caused by genetic predisposition, systemic conditions (such as allergies or illnesses), wounds, or autoimmune reactions to things such as dentures. On occasion it may be considered idiopathic or as having no specific identifiable cause.
Causes
The most usual reason for gingivitis is bacterial plaque surrounding the teeth - the immune system responds to the presence of plaque and this immune response can eventually destroy the gum tissue. It begins with the gums being irritated by plaque and tartar and becoming inflamed around the base of the teeth; which in turn leads them to bleed. This is the cause of gingivitis and if it isn't treated, it becomes periodontitis, alongside further complications, such as tooth loss.
Signs of gingivitis
-
bright red or purple gums that may bleed when brushed/flossed
-
tender gums that may be swollen or painful to the touch
-
halitosis, or malodorous breath
-
receding gums
-
gums that feel soft
In mild cases, people may be unaware of gingivitis because the symptoms are minor; however, even at this stage, it must be taken seriously and addressed straightaway.
Good oral hygiene typically resolves gingivitis: such as brushing more frequently or for longer, alongside flossing and use of antiseptic mouthwash. Plaque and tartar need to be removed through a processed called scaling. Unfortunately, this can be uncomfortable if tartar build-up is widespread or gums are very inflamed and sore.
Periodontitis
Periodontitis is a serious condition that affects the soft tissue (gums) and the bone that supports your teeth; in severe cases, it can mean teeth loosen or even fall out. Research suggests that periodontitis-producing bacteria can enter your bloodstream through the gum tissue and track to organs in your body such as your heart or lungs for example. For this reason, it is thought that periodontitis may underlay respiratory disease, rheumatoid arthritis, coronary artery disease or stroke.
Types of periodontitis
Types of periodontitis differ according to damage of your bone and gingival tissue.
Aggressive periodontitis – once infection caused by bacteria spreads below the gum line, treatment becomes more complicated. Aggressive periodontitis is typified by a rapid deterioration of dental bone and gingival tissue and is one of the directions that periodontitis may progress. At this stage, teeth may appear longer as the gums recede.
Chronic periodontitis – this is the most usual form of the aggressive disease which is distinguished by a more gradual deterioration in bone and gums. At this stage pockets often form in between the gums and teeth and treating this can be challenging.
Periodontitis as a manifestation of a systematic disease – while this is also serious in itself, it is secondary to a more systemic condition, such as diabetes. In diabetes, people are often dehydrated (leading to dry mouth) and the immune system is compromised owing to fluctuations in blood sugar levels. In such cases, gum disease prevention may not have that much of an impact but available treatments options can have an impact on symptoms and slow overall progression of the disease.
Signs of periodontitis
Healthy gums feel firm, appear pale pink and fit securely around the teeth. Signs of periodontitis to watch out for include:
-
bright red or purple gums that may bleed when brushed/flossed
-
tender gums that may be swollen or painful to the touch
-
halitosis, or malodorous breath
-
receding gums or teeth appearing longer
-
Spaces or pockets developing between teeth
-
Discharge or pus between your teeth and gums
-
Wobbly teeth
-
Discomfort when chewing
-
A change in bite (the way your teeth fit together)
The most effective preventative approach to periodontitis is good oral hygiene - one that commences early in life and practiced throughout.
Good oral hygiene. Advise is to brush your teeth for two minutes at least twice a day (morning and night), alongside daily flossing. Flossing is recommended before brushing teeth as loosened food particles and bacteria can then be brushed away.
Regular dental check-ups and cleanings, usually every six to 12 months. Risk factors that increase the likelihood of periodontitis (dry mouth, certain medications or smoking) may necessitate more frequent professional cleans.
- Photo courtesy of SteadyHealth.com
- https://www.ncbi.nlm.nih.gov/books/NBK279593/
- www.ncbi.nlm.nih.gov/pubmed/26281382
- https://www.cdc.gov/oralhealth/periodontal_disease/index.htm
- http://www.jicdro.org/temp/JIntClinDentResOrgan7111-343788_093258.pdf
- www.ijdr.in/article.asp?issn=0970-9290
- year=2018
- volume=29
- issue=2
- spage=254
- epage=259
- aulast=Balaji


Your thoughts on this