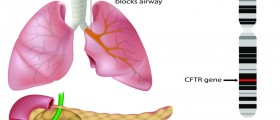
Cystic fibrosis is a disease caused by defects in the cystic fibrosis gene, CFTR. This gene codes the production of a protein that regulates the way chloride passes in and out of cells. There's more than one potential mutation of this gene.
- One mutation results in the complete absence of CFTR protein.
- Another mutation, the most common mutation, known as ΔF508, doesn't completely block the production of this protein, but causes the protein to be made in such a way that it breaks down quickly.
- Yet another mutation of the same gene causes problems in the activation of the protein as the cell stores energy in the form of ATP.
- A fourth possible mutation allows production of the protein, but in a form that it can't do its job very well.
- A fifth possible mutation permits production of the protein in a form that allows it to carry out its functions, but not in the amounts the body needs.
- And a sixth mutation results in changes in the surface of the cell where the protein does its job rather than changes in the protein itself.

In the jargon of genetics, the CTFR gene has poor penetrance. This means that there isn't a very clear relationship between the presence of one mutation or another and the severity of symptoms. This also means that a doctor doesn't know really what to expect just from genetic testing. The problem isn't testing. The problem is the interpretation of tests by doctors who think that symptoms are limited by the results of the test.
Cystic fibrosis is often erroneously considered a "monogenic recessive disease." Monogenic means that defects in just one gene used to be thought to be the cause of the disease. Recessive means that to get cystic fibrosis, someone would have to get one copy of the gene, usually the ΔF508 gene, from both parents.
However, the modern understanding of the disease is that its symptoms aren't due just to the ΔF508 gene that "causes" cystic fibrosis, they are also due to other genes that modify the course of the disease. For example:
- The presence of absence of mutated genes for mannose binding lectin (MBL2) make a difference in how easily the bacteria and fungi that cause lung infections "stick" to the linings of the lungs, and whether or not someone gets an infection and how early in life they start to get infections.
- Variations in the gene for endothelial receptor type A (EDNRA) regulate how sensitive the lungs will be to irritants, the extent to which asthma-like symptoms aggravate cystic fibrosis.
- Transforming growth factor β1 (TGF-β1) regulates how easily the lungs can "remodel" themselves after an infection.
- Many people with cystic fibrosis develop diabetes. This process is regulated by mutations near the gene for transcription factor 7-like 2 (TCF7L2).
- Many people with cystic fibrosis develop liver disease. This process is regulated by the presence or absence of the Z-allele of the α1-antiprotease (SERPINA1) gene.
There are many other genes that are important in cystic fibrosis besides those typically tested. What this means for your treatment is that your doctor needs to be alert to the full range of complications regardless of which of the six most common variations of the "cystic fibrosis" gene you have. It also means that your experience of the disease can be easier than your genetics might predict. There isn't any single gene that tells you that you will have a very difficult life or a relatively easy life (if anything about cystic fibrosis is easy). There is no single test that seals your fate.
Cystic fibrosis is extraordinarily difficult to manage, but cutting edge genetic testing can at least let your doctor and your know what to expect. Just don't settle for a pronouncement of life or death on the basis of a single test.
- Michael R. Knowles and Mitchell Drumm. The Influence of Genetics on Cystic Fibrosis Phenotypes. Cold Spring Harb Perspect Med. 2012 Dec., 2(12):a009548. doi: 10.1101/cshperspect.a009548.
- Photo courtesy of SteadyHealth