i want to know about how nasal air flow can be measured with thermistor
Loading...
This is from a paper by Dr. David Rapoport, M.D., Robert Norman, M.S., R.R.T., and Michael Nielson, R.R.T., R.PSG.T.
The article is titled "Nasal Pressure Airflow Measurement, An Introduction". A pdf of the article can be downloaded at:
http://www.ptservices.com/Downloads/Misc/pdf/primer.pdf
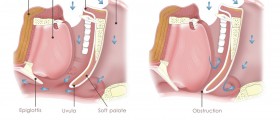
By definition, thermistors and thermocouples are not airflow sensors but are simply detecting the temperature oscillation (between inhaled room air temperature and warmer exhaled air) as a qualitative indicator of airflow. Total cessation of airflow (apnea) is well detected because of the complete lack of temperature variation.
In the mid 1980’s it became clear that it was clinically necessary to detect and count partial airway obstruction events, and the term hypopnea was introduced. Although the original description of hypopnea emphasized significant reductions in airflow it was natural to try to extract this information from thermistors and thermocouples that were in extensive use in most laboratories. However, in the case of incomplete airway obstruction, the relationship between temperature change and true flow is not straightforward. Thus the amplitude of the signal resulting from a partially obstructed breath may be reduced not at all (if the full effect of exhaled warm air is detected) or to a variable extent (depending on characteristics of the sensor and the way in which the signal is processed, e.g., filtered).
Despite the limitations of the thermistor/thermocouple, their use has persisted until recently as the usual clinical practice in most laboratories, and scoring of hypopnea has evolved to the following practice: events of reduced airflow are first identified from the respiratory (thermistor) signal; they are then validated as true hypopneas by their coincidence with desaturation or arousal on EEG. Typical definitions in use today required a decrease in the thermistor signal (50 – 75%) associated with oxyhemoglobin desaturation of 2% – 4% or EEG microarousal. However, if the thermal sensor does not detect a candidate respiratory event and there is no desaturation, arousals are left “unexplained.” As this pattern has been recognized in more symptomatic patients, this has led to the recognition of the Upper Airway Resistance Syndrome (UARS) - defined as the presence of repetitive arousals following periods of increased respiratory effort (detected by esophageal manometry) but undetected by thermal sensors. The degree to which thermistors under-detect respiratory events has recently been investigated. Up to 70% of respiratory events may be missed in patients with symptoms consistent with OSA but without frank apnea/hypopnea. In some cases, the number of events missed with simple thermal technology may be sufficient to alter the ultimate patient diagnosis. A recent position paper from the American Academy of Sleep Medicine (AASM) reemphasized that the detection of reduced airflow (the entry into defining a hypopnea) could not be performed with thermistors or thermocouples and that these devices should be reserved for the detection of apnea only.
The article is titled "Nasal Pressure Airflow Measurement, An Introduction". A pdf of the article can be downloaded at:
http://www.ptservices.com/Downloads/Misc/pdf/primer.pdf
By definition, thermistors and thermocouples are not airflow sensors but are simply detecting the temperature oscillation (between inhaled room air temperature and warmer exhaled air) as a qualitative indicator of airflow. Total cessation of airflow (apnea) is well detected because of the complete lack of temperature variation.
In the mid 1980’s it became clear that it was clinically necessary to detect and count partial airway obstruction events, and the term hypopnea was introduced. Although the original description of hypopnea emphasized significant reductions in airflow it was natural to try to extract this information from thermistors and thermocouples that were in extensive use in most laboratories. However, in the case of incomplete airway obstruction, the relationship between temperature change and true flow is not straightforward. Thus the amplitude of the signal resulting from a partially obstructed breath may be reduced not at all (if the full effect of exhaled warm air is detected) or to a variable extent (depending on characteristics of the sensor and the way in which the signal is processed, e.g., filtered).
Despite the limitations of the thermistor/thermocouple, their use has persisted until recently as the usual clinical practice in most laboratories, and scoring of hypopnea has evolved to the following practice: events of reduced airflow are first identified from the respiratory (thermistor) signal; they are then validated as true hypopneas by their coincidence with desaturation or arousal on EEG. Typical definitions in use today required a decrease in the thermistor signal (50 – 75%) associated with oxyhemoglobin desaturation of 2% – 4% or EEG microarousal. However, if the thermal sensor does not detect a candidate respiratory event and there is no desaturation, arousals are left “unexplained.” As this pattern has been recognized in more symptomatic patients, this has led to the recognition of the Upper Airway Resistance Syndrome (UARS) - defined as the presence of repetitive arousals following periods of increased respiratory effort (detected by esophageal manometry) but undetected by thermal sensors. The degree to which thermistors under-detect respiratory events has recently been investigated. Up to 70% of respiratory events may be missed in patients with symptoms consistent with OSA but without frank apnea/hypopnea. In some cases, the number of events missed with simple thermal technology may be sufficient to alter the ultimate patient diagnosis. A recent position paper from the American Academy of Sleep Medicine (AASM) reemphasized that the detection of reduced airflow (the entry into defining a hypopnea) could not be performed with thermistors or thermocouples and that these devices should be reserved for the detection of apnea only.
Loading...