Table of Contents
Natural Family Planning
First, let's take a look at contraceptive options that women who have perimenopause symptoms or are beyond their mid-forties should not be using. These are the natural birth control techniques that many women use successfully for decades, but that become entirely unreliable when you are transitioning toward the menopause.
Because your periods and ovulation are becoming less frequent, it is simply hard to predict when you ovulate — and therefore also hard to know when you won't be fertile. Cervical mucus also becomes much less reliable when you hit the perimenopause. You may think that your mucus is "non-fertile" and then get pregnant, as indeed happened to someone I know.
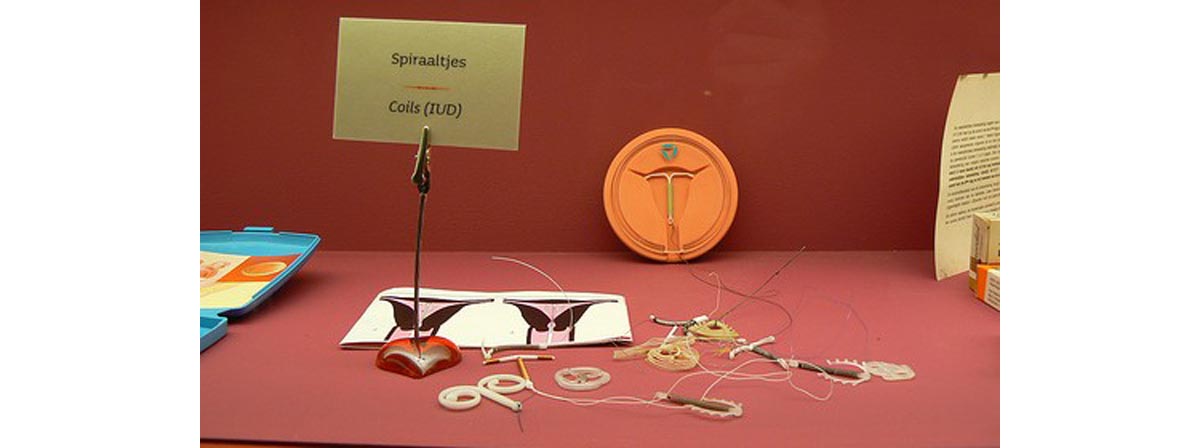
Intrauterine Devices And Tubal Ligation
Intrauterine devices, or IUDs, are much-overlooked contraceptives in the United States. Two forms are on the market in the US: the Paragard IUD and the Mirena intrauterine system. Paragard is a copper IUD that prevents pregnancy for 10 years, while Mirena is a plastic device that also has a hormonal reservoir. The Mirena can be used for five years.
Intrauterine devices are specifically designed for long-term use, and obviously need to be removed when you stop using them.
A less invasive form of "tubal ligation" has now been on the market for some time. Essure and Adiana implants are inserted into the fallopian tubes, where they create a blockage that ensures sperm and egg cannot meet. These methods do not impact hormone levels or menstruation, and the same goes for the more traditional tubal ligation surgery. While these methods are great for older women because they are permanent, they might be too costly to invest in if the menopause is already on the horizon.
Hormonal Contraceptives
Combined oral contraceptives and other combined hormonal contraceptives such as the birth control patch and NuvaRing have pros and cons during the later stages of a woman's reproductive years. Women who are over 35 and smoke less than 15 cigarettes a day should not use combined hormonal contraceptives unless they have no other acceptable option, according to the World Health Organization's Medical Eligibility Criteria (MEC) that govern contraceptive use.
If a woman over 35 smokes more than 15 cigarettes a day, she falls into category four of the MEC — which means she should absolutely not use combined hormonal contraceptives. The risk of myocardial infarction and stroke simply become too high at this point.
There are some pros as well as some cons. The birth control pill essentially acts as a form of Hormone Replacement Therapy, but with a larger dose of hormones. The birth control pill will prevent pregnancy while also reducing the perimenopause symptoms most women struggle with — vaginal dryness, hot flashes, and mood swings.
Now for the con — combined oral contraceptives will give a woman the appearance of regular cycles even when she might already have stopped had she not been using them. Older women who are on the pill can stop using it for a month and have their levels of Follicle-Stimulating Hormone (FSH) checked to see if they have reached the menopause. If you want to have a clear picture of what is going on with your menstrual cycles during the perimenopause, combined hormonal contraceptives are not for you.
Condoms
Condoms are a favorite form of contraception among perimenopausal women because they don't artificially alter hormone levels. Providing they are used correctly, they have a 98 percent success rate.
If you decide to go with condoms, you may want to keep emergency contraceptives at home in case one breaks or slips off. Since perimenopausal women typically experience vaginal dryness, you may also want to add a good lubricant that does not damage latex to your bedroom cupboard.
- Photo courtesy of Kendra Goering by Flickr : www.flickr.com/photos/kendradeann/2790951/
- Photo courtesy of Ryan Somma by Flickr : www.flickr.com/photos/ideonexus/3283049403/

