Dr Chris Pavlinec is an electrocardiologist — a kind of cardiologist who specializes in treating disorders of the heart's electrical system, like arrhythmias. For the past two months, however, his entire department has been dedicated to one thing and one thing only. Chris has been on the frontlines of the battle against the COVID-19 pandemic, mostly treating patients designated as having "mild" cases of the novel coronavirus.
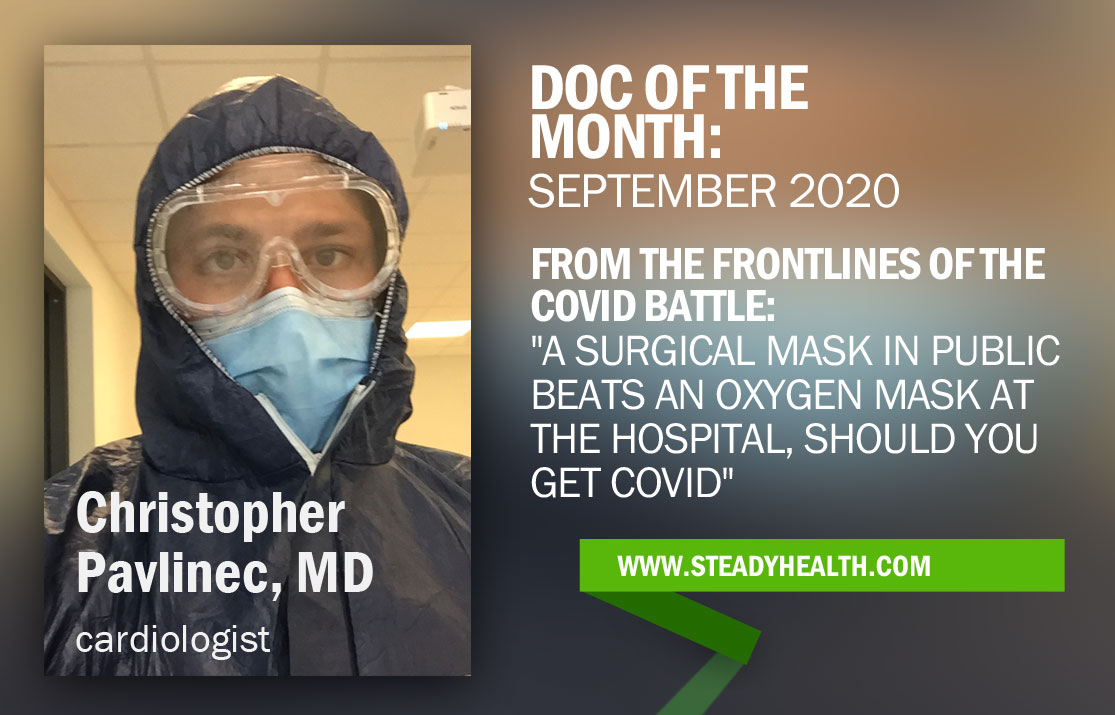
Now, Chris goes to work in personal protective gear reminiscent of the Chernobyl clean-up, getting a much closer and more personal look at the pandemic that has ravaged the world than many of us will ever have the displeasure to.
Even patients hospitalized with mild COVID symptoms 'require constant medical attention'
Have you ever wondered what it really means to be a COVID patient hospitalized with "mild symptoms"? If the word "mild" invokes images of a slight cough and some muscle aches, it misses the mark in this case.
Chris explains:
"These patients do require constant medical supervision. “Mild cases” would be any patient who requires supplemental oxygen or fluid therapy because of symptoms associated with the disease. Many of my patients have oxygen saturation levels below 92 percent, the level that would be considered to be normal in the healthy population.
Without extra oxygen, these patients would be short of breath even after doing simple activities like changing their clothes or walking to the bathroom.
Other patients may also have issues eating or drinking because they suffer from diarrhea or do not have appetites because of the disease. This can easily lead to dehydration and without medical intervention, a certain trip to the Intensive Care Department."
Like most other doctors who treat COVID-19 patients, Chris is, he says, "providing supportive care to make the symptoms more bearable for patients".
There is only so much the medical community can do, and Chris adds: "We can give antibiotics or steroid therapy to prevent patients from requiring respirators, but if after giving oxygen, fluids and these medications we still see that patients are getting worse, we need to transfer them to Intensive Care — because these patients will likely need to be intubated to survive."
'COVID-19 patients can deteriorate to the point of needing a ventilator within a matter of hours'
What message would Chris have for people who brush COVID-19 off as "nothing much to worry about", because they're under the impression that the symptoms are no worse than those of a common cold, or influenza — the true severity of which many also underestimate?
"This is perhaps the most common and frustrating idea that I seemingly address with friends and family who do not know what a typical COVID infection looks like on a daily basis. True, a COVID-19 infection does have symptoms similar to the flu, but the main difference between COVID-19 and influenza is that COVID-19 comes from a zoonotic source. This means that it started as an animal infection that was spread to humans."
The significance of this fact, Chris shares, is that it "makes COVID-19 much harder to treat because the treatments we can currently offer in medicine are designed to attack genetic material from human sources, not animals. This is why patients are not able to quickly recover from the infection."
This has further implications when it comes to treatment, as Chris notes that it's much easier to predict how influenza will impact an individual patient than it is to speculate how COVID will unfold:
"If a patient needs to be hospitalized with a flu infection even in a critical state, there will be a step-wise decline that can usually be reversed with aggressive medical care. Doctors can also plan and coordinate with other departments because the course of the disease is better understood."
COVID-19 is a different beast — and even patients who initially look like they are going to recover without any problems may face an unexpected turn for the worse. Chris warns:
"With COVID infections, most patients have a mild form of the disease for the first week and after about 6 days, they may rapidly decline. I have seen a few cases first-hand where a patient started the morning without requiring oxygen at all, and then deteriorated to the point of needing a respirator to breathe within 6 hours.
When hospitals worldwide are experiencing a shortage of personnel and respirators, this can lead to difficult decisions about who should get a ventilator. These patients also tend to have variable presentations of the disease. Some may have only stomach problems, others just a cough, while some have a combination of simultaneous heart, lung and stomach problems. This makes every case different so we are learning treatment protocols as we go."
COVID-19 also differs from the seasonal flu in another crucially important way, Chris would like to remind SteadyHealth readers — while an annual flu shot can greatly reduce your odds of coming down with influenza, there is no such protection in place against COVID-19.
"Regardless of what news outlets may claim about how close we are to having a vaccine against COVID-19 ready," Chris says, "most of the medical community agrees that the earliest we can hope for a vaccine against COVID-19 will be no sooner than the next 1 to 1.5 years."
When that shot of hope does finally arrive, the coronavirus won't necessarily immediately stop playing a role in daily life. "Even then, we won’t fully know if it is effective or safe so do not be too optimistic about returning to normal life for the next year."
We're still 'unaware of the long-term complications of COVID-19' in younger patients
What would Chris say to younger people who have managed to dodge the virus so far, but don't believe COVID-19 would be that bad if they did get infected?
"Do not fall into a false sense of security that just because you are a certain age, you do not have a risk of experiencing complications from COVID-19. Most of my patients are over the age of 65 but I have recently treated a 32-year-old without any previous health risks. Her symptoms were milder than the average senior citizen’s but she still needed oxygen therapy and had a fever over 39 degrees Celsius during the infection so this can even impact a younger patient."
What about even younger people, like teenagers and children? Chris reminds us that "we are still unaware of long-term complications associated with COVID-19 because this is such a new thing". He adds that some studies suggest that even asymptomatic patients could suffer long-term lung and heart complications, and that "a recent study also claimed a COVID infection could lead to infertility, so until we have a better understanding of COVID, I recommend trying to avoid it through good hygiene and social distancing".
Ultimately, as someone who sees what COVID-19 can do to the human body on a daily basis, Chris wants to caution you against underestimating the virus. "COVID-19 will be more fatal than the flu and we as a medical community still do not have great answers for how to contain it and treat it," he says.
'When your nose is exposed, you are very capable of catching the virus'
Despite the fact that we're all surrounded by COVID-19 related news, and our daily lives are impacted by the pandemic in countless big and small ways, you've still got people who simply can't be bothered to take steps to reduce the risk they and those around them face.
As a doctor, that makes Chris angry.
"When I do get the occasional day off these days, the most infuriating thing that I see walking around my city is how basic prevention measures are being largely ignored by the general public. In my city, most people at least wear masks inside buildings, but about 50 percent are not wearing them properly. People will walk with masks only covering their mouth and leave their nose entirely exposed. I understand that it is not comfortable to wear masks but when your nose is exposed, you are very capable of inhaling or exhaling viral material to spread the infection further.
I can promise you it is far more fun wearing a surgical mask in public than an oxygen mask inside a hospital bed for weeks because of COVID. "
Face masks can play an important role in reducing the spread of the virus, but Chris would also like to urge us not to see them as magic bullets.
"An interesting study I read recently reported that people who wear masks are more likely to catch COVID compared to those who don’t. This may seem strange at first glance, but if you think about it, it may start to become more logical. People wearing masks often think they are invincible against the infection and will forget about other preventative measures."
That can lead to careless behavior, like — Chris says — "walking past hand sanitizer stations without using them, and making no effort to distance themselves from strangers". Some people still "touch surfaces like doors or staircase railings, then grab their phones and take off their masks, crumpling them up into their pockets, the moment they get outside, without ever cleaning their hands".
Chris shares:
"In this anecdote, someone has possibly infected themselves on multiple occasions and if they reuse their mask once they go inside another building, they could be allowing viruses and bacteria easy access to their mouth and nose through their now contaminated mask. People who don’t wear masks at least go out of their way to avoid walking near people and use hand sanitizer often. Although this may seem like paranoia, most doctors would much rather have you do this practice than using a mask improperly."
Venturing outside the safe way, Chris says, would involve taking a few properly packaged surgical masks and a bottle of hand sanitizer with you, and then proceeding to use both correctly. "Once you finish your errands, throw out the mask in a proper waste receptacle and any time you have to touch a door handle or elevator button used by other people, use your hand sanitizer to thoroughly clean your hands. Try to avoid touching the 'T-area' of your face as best as you can as well. This would be between your eyes, nose and mouth. This area represents the most likely vector of infection."
If people continue to protest against coronavirus measures, 'we'll be dealing with COVID-19 for years to come'
The world is beyond ready for this pandemic to be over — but what will the future truly hold? SteadyHealth asked Chris to share his predictions for the coming years.
"COVID-19 is and will be a challenge for the medical community in the coming years for a number of different reasons," Chris told us. One of the main obstacles is "the limited number of resources that hospitals around the globe must deal with", and they mean that doctors just like Chris have to work in an environment short on staff, protective equipment, and ventilators.
Chris paints a picture of what this means in practice when he says:
"In most cases, the care of COVID-19 patients will fall into the hands of specialists who do not have much experience dealing with Intensive Care, Geriatric, or Pulmonology patients. This adds stress to the dynamic and may reduce the quality of care for patients admitted to the hospital. Patients scheduled for appointments also are suffering because their specialists may now be unable to meet with them as departments shift towards the care of COVID-19 patients. There is a backlog of patients waiting for procedures and many fear even going to the hospital because of the risk of catching coronavirus."
What is the best way to handle the risk of COVID-19, then? Some argue in favor of strict social distancing, or secluding ourselves at home until a vaccine is ready for widespread distribution, while others would prefer we carry on with life as if it were 2018, and just dealing with COVID if they catch it — waiting for herd immunity to take care of the problem.
Chris strongly feels that "waiting for a safe and effecive vaccine that may be years away is not a realistic way to approach this disease".
On the other hand, "living without restraints will perhaps help us get through COVID-19 at a faster rate", but Chris warns that because around 10 percent of patients will need to be hospitalized, the health system would be completely overwhelmed. Thousands, and perhaps more, patients would die unnecessarily. They wouldn't just be COVID patients either, but also others in dire need of medical care who won't have doctors to care for them, because the people who might otherwise have saved their life will be busy fighting the pandemic.
The way forward is, then, being fully aware of the potential consequences of a COVID-19 on an indvidual level, and taking all the right steps to reduce your risk. Chris concludes:
"Using good hygiene, social distancing, and wearing masks in public places is the best way to handle the pandemic. These measures will help reduce the spread of the infection and allow us to have a semblance of the normal life we were used to before the coronavirus.
In a perfect world, with personal preventative measures put in place, I am optimistic that we may move past COVID-19 by the end of 2021. If populations around the globe continue to protest against wearing masks in public or view the coronavirus as something comparable to the flu, however, many more people will die and we will be dealing with the coronavirus for years to come."
- Photo courtesy of Chris Pavlinec/SteadyHealth


Your thoughts on this