While the causes are many; the most common cause for a severely swollen, painful, itchy, and inflamed vaginal area is a condition called Vulvovaginitis, which is characterized by chronic inflammation and/or infection of the vulva and the vagina.
Symptoms
- Intolerable itching and irritation in the genital area
- Vaginal discharge that can be heavy, thick, green, grey, or yellow
- Inflammation, swelling, redness, and irritation of the labia majora, the labia minora, and/or the perineal area
- Fishy or foul vaginal odor
- Pain, discomfort , and burning while urinating

Causes of Vulvovaginitis
The condition, Vulvovaginitis is quite common and no woman is immune to it. It affects women of all ages and backgrounds. The condition is often triggered or caused by:
- Bacteria, parasites, viruses, and yeasts, and certain sexually transmitted infections (STIs).
- Poor hygiene, allergens, fragranced soaps, bath gels, perfumes, feminine products, vaginal contraceptives, that can cause itching, rashes and inflammation in the genital area.
- Tight-fitting, non-absorbent clothing that can cause irritation and heat rashes. Especially since irritated skin tissue is more prone to infection than normal and healthy skin issue.
- Wet clothing, unclean, or damp undergarments provide perfect breeding grounds for infection-causing organisms , since they thrive in dark, warm , moist environments. Such conditions are guilty of not just causing the Vulvovaginitis; but they can also prolong its period.
- Bacterial vaginosis: Is another cause and is an overgrowth of certain types of bacteria within the vagina. Such bacteria are also responsible for a thin, grey-like vaginal discharge and a very fishy vaginal odor.
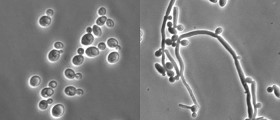
- Candida albicans: Is famous for causing yeast infections and are perhaps the most common causes of Vulvovaginitis in women. Yeast infections usually start off with itching in the genital area, as well as with a thick cottage-cheese type white discharge, and can become quite inflamed and swollen and can lead to other symptoms if left untreated.
- It is also important to be aware of the fact that the use of antibiotics can also cause yeast infections, since they tend to kill the normal anti-fungal bacteria inside the vagina.
- Trichomonas vaginitis: Is a sexually transmitted infection, and another very common cause of Vulvovaginitis. It is characterized by major itching in the genital area, a strong, usually unpleasant vaginal odor and a heavy discharge, which is sometimes yellow, grey or green.
- Vulvovaginitis is also common in post-menopausal women due to the drop in their estrogen levels, which usually causes vaginal dryness, thinning of the vaginal walls and tissues and can lead to even more aggressive genital inflammation, burning and itching.
- Certain skin conditions, lost or 'forgotten' tampons, and even puberty (since the vagina is not as acidic then), poor hygiene, fecal bacteria from wiping anal to vaginal.
- Sexual abuse especially in young girls (from Gonorrhea-related vaginitis), can all lead to recurrent and unexplained episodes of ongoing chronic inflammation and itching of the vulva.
Words of Caution
While many women will try over the counter medication such as Monistat for yeast infections, since many conditions mimic others(have the same /similar symptoms) bear in mind that if the symptoms still persist after a week, this could be the sign of something else, and you should see your doctor immediately.
Your doctor can and will then perform a pelvic examination, and be able to detect any inflammation, swelling, and redness on the vagina or vulva. Depending on your doctor's professional opinion and diagnosis; he or she will prescribe a course of treatment that could include medications such as: oral or topical (skin) antibiotics; anti-fungal cream; estrogen cream for women with low levels; steroidal creams such as cortisone; and antihistamines for allergic reactions.
He or she will also recommend daily precautions regarding the proper types of underwear and clothing and ways you can decrease moisture and increase oxygen and proper air flow into the genital area. It is also important to be aware that if in fact you have been diagnosed with a STI, to prevent reinfection, it is critical that your sexual partner(s) be treated as well, and even if they have no physical symptoms or signs. As always, be smart-play it safe. Take your health into your own hands.
- Photo courtesy of SteadyHealth