How does MS cause anxiety?
Multiple sclerosis (MS) is a chronic autoimmune disease which affects the central nervous system. The cause for the condition is unclear although a multitude of factors are implicated, including both genetic and environmental aspects. There is no cure for MS although an holistic approach typically involving neuro-rehabilitation, drug treatments and symptom management approaches can make significant inroads into its impact. MS exists in both relapsing and progressive forms; the vast majority of people are diagnosed with relapsing MS. Relapses can occur seemingly without any obvious trigger and present as sudden deterioration of symptoms with full or partial recovery over the subsequent weeks or months.
However, the anxiety in MS, does not appear to be part of the physical disease (according to MRI scans), but rather originates from the realities of living with the condition. Being able to plan your life without knowing what the effects of MS may be on it from one moment to the next is unsurprisingly a key trigger.
Lack of awareness about the condition also often increases anxieties felt by the newly diagnosed. As a result, often, when faced with a life-limiting illness, people often concentrate on their physical health and so can neglect their emotional wellbeing. This lack of attention can unfortunately result in transient mental health states becoming pathological and moving into the territory of a disorder.
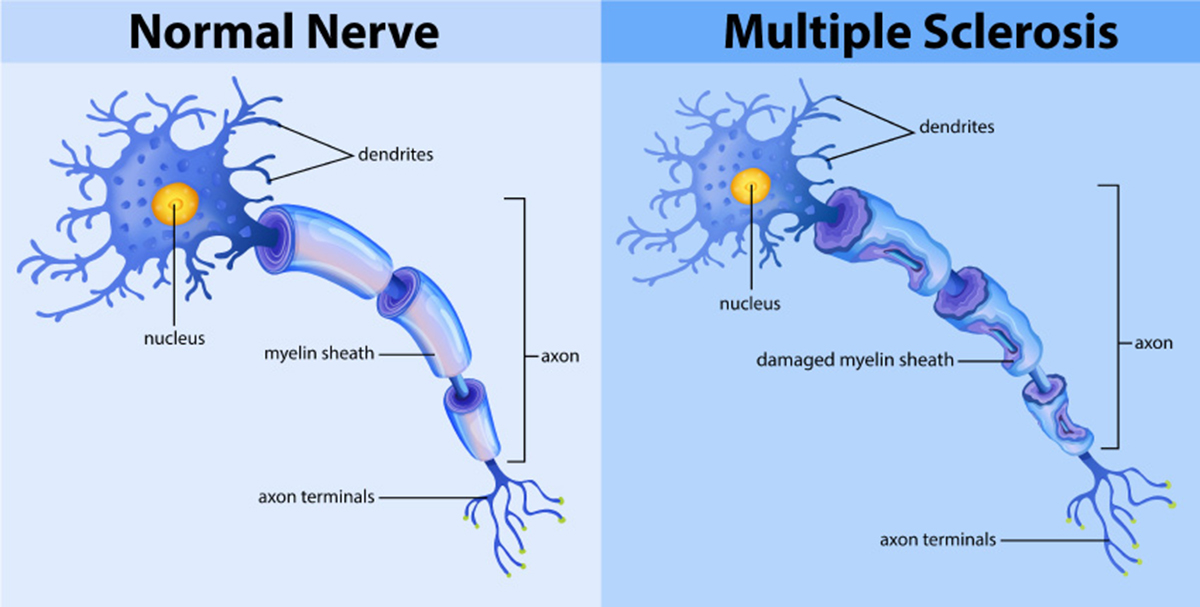
In addition to emotional and psychological reactions to diagnosis, demyelination and damage to nerve fibers in the brain can cause emotional changes too. Furthermore, some of the medications (specifically steroids) prescribed can also impact upon mental health in many challenging ways.
Prevalence of anxiety in the MS population
Studies indicate that there is a strong relationship between physical disability and anxiety, that physical disability affects anxiety differently, and that these effects differ according to gender, age, disease course and disease duration. Several studies have found that MS itself is a strong predictor of anxiety (and depression), and that other factors may mask the full extent of this effect so it may be even greater than research has been able to show.
The literature indicates that anxiety levels peak at onset of the condition and when it is comorbid with depression; social isolation and misuse of alcohol can also increase the risk of anxiety being present. Sadly, the combination of anxiety and depression in MS can also lead to higher rates of suicide amongst this group if their mental health needs remain unaddressed.
How does stress or anxiety affect MS?
Exposure to stress has for some time been suspected as a factor that can aggravate MS. There are many studies showing that among people diagnosed with MS, stressful life events are associated with a significant increase in risk of MS exacerbation in the weeks or months following onset of the stressor But it is not known whether stressful life events could increase the risk of developing the disease itself.
Treatment of Anxiety in MS
As we can see, it is crucial that the emotional and psychological aspects of this condition do not get ignored. Apart from the interrelationship between these factors and physical health meaning that anxiety can trigger a worsening of the condition, the risk of suicide is one not to be taken lightly. Mental wellbeing is also known to influence an individual's compliance with treatment so attention to psychological factors is of concern to all.
The challenge with all co-existing conditions is how to detect them and how should they be treated? The traditional psychotherapeutic approaches to anxiety, for example, may be highly inappropriate when MS is present. For example, in the absence of a life-limiting illness, the treatment might be focusing on challenging disproportionate or unrealistic fears; however in MS, the threat that the condition poses is very real.
Symptoms of anxiety in MS are no different to those in a healthy individual; however, unfortunately, they are often overlooked and misattributed to the disease.
When a mental health condition is suspected alongside a physical health problem, specific psychometric measures will often be used to facilitate detection. In the case of anxiety and MS, the following questionnaires may be used:
-
The Hamilton Anxiety Scale (HAS)
-
Hospital Anxiety and Depression Scale (HAD)
-
State-Trait Anxiety Inventory (STAI)
The complication can be where depression is also present as this can mask the anxiety; or, in older people, anxiety can often mask depression.
Often therapeutic work needs to focus on the person re-evaluating their sense of self, which will have been catastrophically altered in the light of their diagnosis. As the condition progresses, different challenges and new uncertainties must be faced, leading to constant re-evaluation, readjusting, coping with loss.This may trigger new episodes of anxiety which need equal attention. For example, some may be diagnosed initially with a relapsing form of MS but then be later told they have the progressive form which can feel like being re-diagnosed all over again.
‘Talking therapies’ such as cognitive behavioral therapy (CBT) or mindfulness-based approaches are believed to be helpful in enabling people to cope better and reduce their symptoms of anxiety. CBT works by encouraging people to examine how their thoughts and feelings affect how they behave. Often people become entrenched in dysfunctional patterns of thinking, especially if they are feeling anxious. CBT enables people to develop different ways of thinking so they can, in turn, change the way they feel and behave.
Individuals may also be encouraged to reduce anxiety more generally by learning various stress-reduction techniques such as:
-
Being aware of and challenging “black or white thinking”; alongside avoiding catastrophic thinking.
-
Lifestyle changes such as trying to exercise wherever possible.
-
Breaking down fears into manageable and achievable problem-solving tasks in the here-and-now.
-
Acknowledging and normalizing feelings that are proportionate to the disease, while facilitating the expression of grief and loss.
Other approaches that may be used include SSRI antidepressants and biofeedback (a technique that teaches the control of bodily responses) as well as spiritual approaches such as meditation.
- mymsaa.org/ms-information/symptoms/anxiety/
- www.nationalmssociety.org/Symptoms-Diagnosis/MS-Symptoms/Emotional-Changes
- www.ncbi.nlm.nih.gov/pmc/articles/PMC3115807/
- www.ncbi.nlm.nih.gov/pmc/articles/PMC4143231/
- www.ncbi.nlm.nih.gov/pmc/articles/PMC4143231/
- Michalski D, Liebig S, Thomae E, Singer S, Hinz A, Bergh FT., Anxiety, depression and impaired health-related quality of life are therapeutic challenges in patients with multiple sclerosis.Ment Illn. 2010 Jan 25, 2(1):e5
- Jones KH, Ford DV, Jones PA, John A, Middleton RM, Lockhart-Jones H, Osborne LA, Noble JG., A large-scale study of anxiety and depression in people with Multiple Sclerosis: a survey via the web portal of the UK MS Register. PLoS One. 2012, 7(7):e41910
- www.nursinginpractice.com/article/tackling-anxiety-people-multiple-sclerosis
- Photo courtesy of SteadyHealth.com


Your thoughts on this